April 2015 | VOL. 14, NO. 4 | www.McGowan.pitt.edu
From Bench to Bedside: Technology Developed by McGowan Faculty Used in Clinical Setting
 Based on core technology developed by McGowan Institute of Regenerative Medicine faculty members William Federspiel, PhD, W.K. Whiteford professor of bioengineering, chemical engineering, and critical care medicine, and the late Brack Hattler, MD, ALung Technologies developed a product called the Hemolung Respiratory Assist System (RAS) which is a dialysis-like alternative or supplement to mechanical ventilation. The Hemolung RAS was implanted into the first person in the U.S. at the University of Pittsburgh Medical Center (UPMC). The device was used as a bridge to transplantation upon receiving the U.S. Food and Drug Administration’s approval to use the technology on a compassionate use basis. The Hemolung story is a great example of moving university research from the laboratory to the market to make the world a better place and is the focus of this latest video.
Based on core technology developed by McGowan Institute of Regenerative Medicine faculty members William Federspiel, PhD, W.K. Whiteford professor of bioengineering, chemical engineering, and critical care medicine, and the late Brack Hattler, MD, ALung Technologies developed a product called the Hemolung Respiratory Assist System (RAS) which is a dialysis-like alternative or supplement to mechanical ventilation. The Hemolung RAS was implanted into the first person in the U.S. at the University of Pittsburgh Medical Center (UPMC). The device was used as a bridge to transplantation upon receiving the U.S. Food and Drug Administration’s approval to use the technology on a compassionate use basis. The Hemolung story is a great example of moving university research from the laboratory to the market to make the world a better place and is the focus of this latest video.
The Patient’s Story
TSuffering from cystic fibrosis and rejecting the transplanted lungs he had received just 2 years ago, Jon Sacker, 33, came to UPMC from his hometown in Moore, Oklahoma, as a last resort. But when his carbon dioxide levels spiked, making him too sick for another transplant, his family feared the worst.
“I thought I had brought my husband here to die,” said Mr. Sacker’s wife, Sallie.
Instead, UPMC clinicians turned to a Pittsburgh-made device called the Hemolung RAS that would filter out harmful carbon dioxide and provide healthy oxygen to his blood, giving Mr. Sacker a chance to gain enough strength to undergo a lifesaving transplant. He became the first person in the U.S. to be implanted with the Hemolung RAS. After 20 days on the Hemolung, his condition improved to the point that he underwent a double lung transplant and today is on the road to recovery.
“The entire series of events that led to this transplant and Jon’s recovery have been amazing,” said McGowan Institute for Regenerative Medicine faculty member Christian Bermudez, MD, chief of UPMC’s Division of Cardiothoracic Transplantation. “Jon had previously been very active and fit, and we knew we had to do whatever it took to help him.”
“Jon was in very critical condition when he came to Pittsburgh, and the Hemolung was a lifesaver for him while waiting for his second lung transplant. We are very proud of his good recovery,” said Mr. Sacker’s pulmonologist, Mario Crespo, MD, associate medical director of UPMC’s Lung Transplant Program.
The Hemolung Development Story
Several years before, Dr. Federspiel, director of the Medical Devices Laboratory at the McGowan Institute for Regenerative Medicine, along with a designer fabricator and a bioengineering doctoral student, developed what was known as the Paracorporeal Respiratory Assist Lung. The device underwent product development and was commercialized by ALung Technologies as the renamed Hemolung RAS. ALung was based on the technology developed by Dr. Federspiel and UPMC’s former chief of lung transplantation, Dr. Hattler, MD.
Many patients waiting for lungs or a heart use mechanical devices as a bridge to transplant. But doctors said Mr. Sacker was too sick for the traditional extracorporeal membrane oxygenation, or ECMO. However, UPMC doctors knew about the Hemolung RAS, which removes carbon dioxide and delivers oxygen directly to the blood, allowing a patient’s lungs to rest and heal.
“We had seen the Hemolung RAS used in other countries and wanted to do whatever we could to help this patient,” said Peter M. DeComo, chairman and chief executive of ALung Technologies.
Emergency Approval for Use
Drs. Bermudez and Crespo worked with Diana Zaldonis, MPH, BSN, in UPMC’s Division of Cardiac Surgery, to request approval from the Food and Drug Administration officials to use the Hemolung RAS for this case, as no other alternative therapy was available. At this time the Hemolung RAS isn’t approved for use in the U.S. Meanwhile, Mr. DeComo drove with another ALung official in the middle of the night to Toronto, where the closest Hemolung RAS was available.
“What we do as scientists at Pitt is we develop technology. In order to get that into patients, that technology has to be translated into what’s called a product. Universities just don’t have that capability,” said Dr. Federspiel. “So I feel that a life was saved. A lot of people deserve credit for developing a safe and very effective medical device that can treat patients like Jon.”
RESOURCES AT THE MCGOWAN INSTITUTE
May Special at the Histology Lab
Elastin is a protein in connective tissue that is elastic and allows many tissues in the body to resume their shape after stretching or contracting. Elastin helps skin to return to its original position when it is poked or pinched.
Elastin serves an important function in arteries as a medium for pressure wave propagation to help blood flow and is particularly abundant in large elastic blood vessels such as the aorta. Elastin is also very important in the lungs, elastic ligaments, the skin, and the bladder, elastic cartilage. It is present in all vertebrates above the jawless fish.
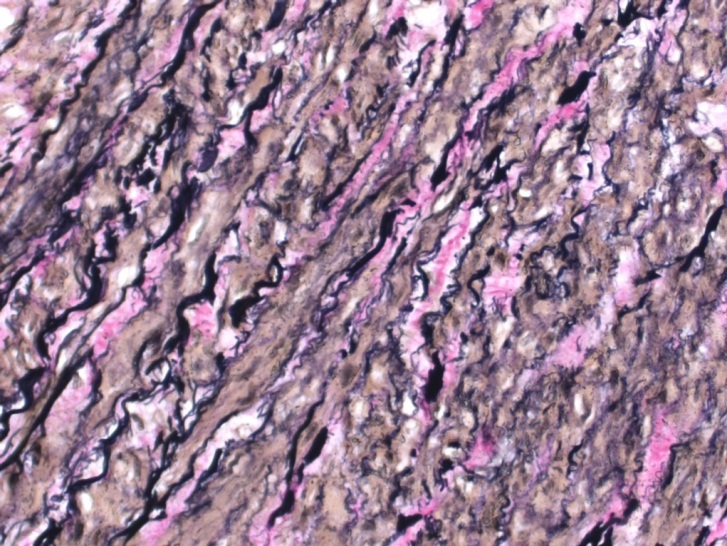
Verhoeff’s stain forms a variety of cationic, anionic and non-ionic bonds with elastin, the main constituent of elastic fiber tissue. Elastin has a strong affinity for the iron-hematoxylin complex formed by the reagents in the stain and will hence retain dye longer than other tissue elements. This allows elastin to remain stained, while remaining tissue elements are decolorized. Elastic fibers and cell nuclei are stained black, collagen fibers are stained red, and other tissue elements including cytoplasm are stained yellow.
You’ll receive 30% off your VVG stain every day in May.
Contact Lori at the McGowan Core Histology Lab and ask about our VVG specials. Email perezl@upmc.edu or call 412-624-5265.
As always, you will receive the highest quality histology in the quickest turn-around time.
Did you know the more samples you submit to the histology lab the less you pay per sample? Contact Lori to find out how!
UPCOMING EVENTS
5th Annual International Vision Conference
 The 5th Annual Conference on Vision Restoration: Regenerative Medicine in Ophthalmology will be held on June 25 – 26, 2015 in Pittsburgh, PA.
The 5th Annual Conference on Vision Restoration: Regenerative Medicine in Ophthalmology will be held on June 25 – 26, 2015 in Pittsburgh, PA.
This conference brings together 150+ multidisciplinary experts including scientists, clinicians, engineers, and others working in the fields of Ophthalmology and Regenerative Medicine. Attendees will be able to share ideas, insights and discoveries that will improve the outcomes for the vision impaired.
University Club
(located on the University of Pittsburgh Campus)
123 University Place
Pittsburgh, PA 15260
For more information, please contact Lauren Wally at (412) 864-3283 or wallyl@upmc.edu.
Fourth Annual Regenerative Rehabilitation Symposium
 The annual Regenerative Rehabilitation Symposia series is a unique opportunity for students, researchers, and clinicians working in the interrelated fields of regenerative medicine and rehabilitation to meet, exchange ideas, and generate new collaborations and clinical research questions. Jointly organized by the University of Pittsburgh Rehabilitation Institute, the School of Health and Rehabilitation Sciences at the University of Pittsburgh, the McGowan Institute for Regenerative Medicine and the Rehabilitation Research and Development Center of Excellence at the Veterans Affairs Palo Alto Health Care System, the Fourth Annual Symposium on Regenerative Rehabilitation will be held on September 24-26, 2015 in Rochester, MN, hosted by the Mayo Clinic.
The annual Regenerative Rehabilitation Symposia series is a unique opportunity for students, researchers, and clinicians working in the interrelated fields of regenerative medicine and rehabilitation to meet, exchange ideas, and generate new collaborations and clinical research questions. Jointly organized by the University of Pittsburgh Rehabilitation Institute, the School of Health and Rehabilitation Sciences at the University of Pittsburgh, the McGowan Institute for Regenerative Medicine and the Rehabilitation Research and Development Center of Excellence at the Veterans Affairs Palo Alto Health Care System, the Fourth Annual Symposium on Regenerative Rehabilitation will be held on September 24-26, 2015 in Rochester, MN, hosted by the Mayo Clinic.
For more information on this event, please contact Katy Wharton at: rehabmtg@pitt.edu or whartonkm@upmc.edu or call 412-624-5293.
SCIENTIFIC ADVANCES
Bioresorbable Metals in Regenerative Medicine
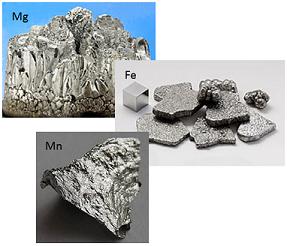 Researchers from the McGowan Institute for Regenerative Medicine and the University of Pittsburgh’s Swanson School of Engineering are creating biodegradable tissue repair structures for the human body as well as developing degradable magnesium (Mg) alloys for craniofacial and orthopedic applications.
Researchers from the McGowan Institute for Regenerative Medicine and the University of Pittsburgh’s Swanson School of Engineering are creating biodegradable tissue repair structures for the human body as well as developing degradable magnesium (Mg) alloys for craniofacial and orthopedic applications.
McGowan Institute for Regenerative Medicine affiliated faculty member Prashant Kumta, PhD, the Swanson School’s Edward R. Weidlein Chair Professor and professor of bioengineering, chemical and petroleum engineering, mechanical engineering and materials science, and professor of oral biology in the School of Dental Medicine, is the principal investigator of the America Makes project entitled “Additive Manufacturing of Biomedical Devices from Bioresorbable Metallic Alloys for Medical Applications.” Dr. Kumta was recently interviewed by Bridget Butler Millsaps of 3DPrint.com about how his lab is using 3D printing to produce microscopic scaffolds of iron (Fe) and manganese (Mn) alloys to foster new bone and tissue growth.
Using a Fe-Mn combination, Dr. Kumta has discovered a 3D printed material that corrodes more effectively and rapidly. It has also been verified as a viable solution in pre-clinical studies due to a 3D printed mandible researchers were able to produce working from a CT scan. The research study is promising because it shows that indeed these scaffolds are significantly similar to those of bone and allow for good “cell viability” as well as “cell infiltration.”
“What makes our materials unique is that we are printing novel proprietary alloys that are biodegradable,” Dr. Kumta told 3DPrint.com.
With metals offering greater durability and success than plastics or polymers for artificial scaffolding, this has led researchers to give attention to attempting its use in 3D printing and use for tissue regeneration. With the Fe-Mn combination, all the required elements come together for density, mechanical properties, as well as the required porous qualities for widespread tissue formation.
“The proprietary Fe based alloys that have already been printed by our binder jetting printing approach is unique and demonstrates faster and improved degradation,” Dr. Kumta said. “Similarly, we are showing demonstration of ability to print novel proprietary Mg based alloys also by the binder jetting printing approach… Both of these examples of novel alloys fabricated into 3-D constructs using our Additive Manufacturing approach are unique.”
As published recently in Acta Bacterialia by authors Dr. Kumta and McGowan Institute for Regenerative Medicine affiliated faculty members Konstantinos Verdelis, DDS, PhD, assistant professor of restorative dentistry/comprehensive care, School of Dental Medicine, Bernard J. Costello, MD, DMD, professor, chief/h3ision of craniofacial and cleft surgery, and Charles Sfeir, DDS, PhD, associate dean of research in the School of Dental Medicine, an associate professor in the Clinical and Translational Science Institute, an associate professor in the Schools of Dental Medicine and Engineering, and the founding director of the Center for Craniofacial Regeneration—each year millions of Americans suffer bone fractures, often requiring internal fixation. Current devices, like plates and screws, are made with permanent metals or resorbable polymers. Permanent metals provide strength and biocompatibility, but cause long-term complications and may require removal. Resorbable polymers reduce long-term complications, but are unsuitable for many load-bearing applications. To mitigate complications, degradable Mg alloys are being developed for craniofacial and orthopedic applications. Their combination of strength and degradation make them ideal for bone fixation.
In accordance with the team’s pre-clinical study, they observed bone formation surrounding 99.9% Mg devices in an ulna fracture model, with fracture healing by 8 weeks and complete overgrowth by 16 weeks. Device degradation, fracture healing, and bone formation were evaluated using microcomputed tomography, histology, and biomechanical tests. Bend tests revealed no difference in flexural load of healed ulnae with Mg devices compared to intact ulnae. These data suggest that Mg devices provide stabilization to facilitate healing, while degrading and stimulating new bone formation.
Illustration: Wikipedia.
Metabolic Disorder Treatment Through Liver Cell Transplant
 Management of patients with hepatic failure and liver-based metabolic disorders is complex and expensive. Hepatic failure results in impaired coagulation, altered consciousness and cerebral function, a heightened risk of multiple organ system failure, and sepsis. Liver transplantation is often the only available treatment option for severe, even if transient, hepatic failure. Patients with life-threatening liver-based metabolic disorders similarly require organ transplantation even though their metabolic diseases are typically the result of a single enzyme deficiency, and the liver otherwise functions normally.
Management of patients with hepatic failure and liver-based metabolic disorders is complex and expensive. Hepatic failure results in impaired coagulation, altered consciousness and cerebral function, a heightened risk of multiple organ system failure, and sepsis. Liver transplantation is often the only available treatment option for severe, even if transient, hepatic failure. Patients with life-threatening liver-based metabolic disorders similarly require organ transplantation even though their metabolic diseases are typically the result of a single enzyme deficiency, and the liver otherwise functions normally.
More than 17,000 patients currently await liver transplantation in the United States, a number that seriously underestimates the number of patients that need treatment, as it has been estimated that more than a million patients in the United States could benefit from transplantation. Unfortunately, use of whole liver transplantation to treat these disorders is limited by a severe shortage of donors and by the risks associated with major surgery. Hepatocyte transplantation holds great promise as an alternative to organ transplantation for the treatment of liver diseases, and numerous pre-clinical studies indicate that transplants consisting of isolated liver cells can correct various metabolic deficiencies of the liver and can reverse hepatic failure.
The study transplant procedure headed by Ira Fox, MD (director of the Center for Innovative Regenerative Therapies – a collaborative effort between the Children’s Hospital of Pittsburgh of UPMC and the McGowan Institute for Regenerative Medicine – and a professor of surgery at the University of Pittsburgh School of Medicine), which involves injection of isolated hepatocytes into the liver through the portal vein, is far less intrusive than transplantation of the whole liver and could be performed on severely ill patients with relatively low risk. In the presence of normal host liver architecture, the transplanted cells integrate into the host liver, providing considerable restorative potential. Because the native liver is not removed, the transplanted hepatocytes need only improve some of the functions of the failing liver and need not replace all hepatic functions.
Although clinical trials of hepatocyte transplantation have demonstrated the long-term safety of the procedure, only partial correction of metabolic disorders has been achieved, and the degree to which donor hepatocytes have restored failing livers has not been adequate to circumvent the need for organ replacement.
As reported by Jessica Wapner, Scientific American, hepatocyte transplantation could treat an estimated half of the metabolic disorders currently indicated for liver transplants, replacing “perhaps up to 10 percent of pediatric transplant candidates,” Dr. Fox says, along with many adult patients. Anyone living with phenylketonuria (PKU)—the disorder occurs in about 1 of every 15,000 newborns in the U.S.—could also benefit. The most common indications for adult liver transplant, cirrhosis-induced liver failure and hepatitis C, cannot be treated by cell-only transplantation because the abnormal structure of the diseased organ will not allow new cells to survive.
Donor Supports Research Addressing Dupuytren’s Disease
 The McGowan Institute for Regenerative Medicine recently received a $100,000 gift in support of the vital work being done by Latha Satish, MSc, MPhil, PhD. As a Research Assistant Professor in the Department of Plastic Surgery at the University of Pittsburgh, Dr. Satish’s research is focused primarily on gaining a better understanding of the pathology and progression of Dupuytren’s disease (DD). Dupuytren’s disease is a complex, progressive, fibroproliferative disorder of the palmar fascia (a thin sheet of connective tissue in the palm of the hand) that results in the shortening, thickening, and fibrosis of the fascia and aponeurosis of the palm. Dr. Satish’s research is focused both at the cellular and molecular level and aims to identify new therapeutic strategies to effectively prevent the progression and recurrence of this disease.
The McGowan Institute for Regenerative Medicine recently received a $100,000 gift in support of the vital work being done by Latha Satish, MSc, MPhil, PhD. As a Research Assistant Professor in the Department of Plastic Surgery at the University of Pittsburgh, Dr. Satish’s research is focused primarily on gaining a better understanding of the pathology and progression of Dupuytren’s disease (DD). Dupuytren’s disease is a complex, progressive, fibroproliferative disorder of the palmar fascia (a thin sheet of connective tissue in the palm of the hand) that results in the shortening, thickening, and fibrosis of the fascia and aponeurosis of the palm. Dr. Satish’s research is focused both at the cellular and molecular level and aims to identify new therapeutic strategies to effectively prevent the progression and recurrence of this disease.
Currently there is no treatment available that can successfully cure or to prevent the recurrence of DD. The development of better therapies has been slowed in part by the lack of an animal model in which candidate therapies may be initially assessed. Unique to humans, DD does not have a counterpart in the animal kingdom, making things much more difficult. Prior to the recent philanthropic gift, Dr. Satish’s team attempted a nine-week study to create an animal model of DD by using athymic “nude” rats to investigate the characteristics of human fibroblasts transplanted into an immunodeficient animal host. The goal was to see if these fibroblasts could maintain their distinct disease phenotype compared to control cells harvested from the fascia of individuals undergoing carpal tunnel release. Through this, DD-derived fibroblasts showed greater persistence over time than control carpal tunnel (CT) – derived fibroblasts, and retained a distinct pro-fibrotic physiology.
However, while there was molecular and histological evidence of building fibrosis with DD cells, there was no development of a frank tissue contracture similar to the clinical presentation in humans. This is potentially due to the fact that the model did not completely mimic the human pathophysiology or because more time was required for that degree of fibrosis and contracture to become established. Since Dupuytren’s is a disease with a slow and progressive onset, it often takes years to become clinically significant.
Thanks to a generous donor, Dr. Satish can now begin a new, more extensive study. This time, animals injected with the DD cells will be allowed to persist in situ for even longer periods of time. Because even DD cells do show some element of decline over time, Dr. Satish will perform repeated doses of DD cells to achieve frank tissue contracture. Simultaneously, the previous model that showed increased evidence of fibrosis with DD cells in comparison to CT cells will be used to test novel therapeutic test agents. Any agent found to diminish the DD-dependent fibrotic characteristics (eg. reduction in the levels of ECM proteins, namely collagen; ability to reduce contraction, etc.) will be a potential candidate for clinical translation. To accomplish these goals Dr. Satish collaborates with clinicians Sandeep Kathju MD, PhD, Department of Plastic Surgery and Mark E Baratz MD, Department of Orthopedic Surgery of University of Pittsburgh.
For more information on how you can support this important work, please contact Sam McCrimmon at mccrimmonsi@upmc.edu or 412-647-1434.
Physical Therapy, Surgery Produce Same Results for Stenosis in Older Patients
 Symptoms from lumbar spinal stenosis, an anatomical impairment common with aging, were relieved and function improved in as many patients utilizing physical therapy as those taking the surgical route, McGowan Institute for Regenerative Medicine affiliated faculty member Anthony Delitto, PhD, and University of Pittsburgh researchers discovered in a 2-year study published in Annals of Internal Medicine.
Symptoms from lumbar spinal stenosis, an anatomical impairment common with aging, were relieved and function improved in as many patients utilizing physical therapy as those taking the surgical route, McGowan Institute for Regenerative Medicine affiliated faculty member Anthony Delitto, PhD, and University of Pittsburgh researchers discovered in a 2-year study published in Annals of Internal Medicine.
It is the first study that clearly compared outcomes between surgery and an evidence-based, standardized physical therapy approach for lumbar spinal stenosis. The condition, created by a narrowing of the spinal canal that puts pressure on the nerve roots resulting in pain, numbness, and weakness through the back and lower extremities, has caused decompression surgery to become the fastest-growing intervention in today’s older population.
A total of 169 patients aged 50-plus already headed for decompression surgery agreed to be randomly assigned into two groups: Those who would have the procedure, and those who went through two standardized, evidence-based physical therapy sessions per week for 6 weeks. After both groups were re-examined at intervals of 6 months, 1 year, and 2 years, the patient outcomes appeared to be equal. There were no detectable differences between the groups in how their pain abated and the degree to which function was restored in their backs, buttocks, and legs.
“Probably the biggest point to put across to physicians, patients, and practitioners is: Patients don’t exhaust all of their non-surgical options before they consent to surgery. And physical therapy is one of their non-surgical options,” said principal investigator Dr. Delitto, chair of the Department of Physical Therapy, Pitt School of Health and Rehabilitation Sciences (SHRS), as well as a member of Pitt’s Health Policy Institute (HPI), and a consultant to UPMC.
Dr. Delitto, a physical therapist, and his SHRS colleagues have long puzzled over why some patients reacted well to physical therapy (PT) and others to surgery.
“The idea we had was to really test the two approaches head to head,” he said. “Both groups improved, and they improved to the same degree. Now, embedded in that, there are patients who did well in surgery, and patients who failed in surgery. There are patients who did well in PT, and there are patients who failed with PT. But when we looked across the board at all of those groups, their success and failure rates were about the same.”
The research project also revealed issues surrounding PT appointments and the cost of co-pay, which may prove enlightening to policymakers enmeshed in the charged atmosphere around health care, Dr. Delitto added.
Most patients didn’t finish the PT regimen allowed them under Medicare and prescribed by the researchers, and one-third of the patients failed to complete even half of the regimen. Another 16 percent didn’t show for a single treatment, though they had agreed to consider PT.
“One of the big things that we know held patients back from PT were co-payments,” Dr. Delitto added. “Patients were on Medicare, and a lot of them were on fixed incomes. Some of those co-payments had to come out of pocket at $25, $30, $35 per visit. That adds up, and some of the patients just couldn’t afford it.”
Illustration: UPMC
Vanderbilt and Pittsburgh to Lead New Center to Identify Toxic Chemicals
 Each day we are bathed in thousands of man-made chemicals that never existed in nature. They are in cosmetics and shampoo, food packaging and plastic containers, clothing and building materials, furniture and electronic devices.
Each day we are bathed in thousands of man-made chemicals that never existed in nature. They are in cosmetics and shampoo, food packaging and plastic containers, clothing and building materials, furniture and electronic devices.
Although the U.S. now produces more than 500 million tons of synthetic chemicals annually, a major “toxicological information gap” has developed regarding the risks they pose to human health and the environment. According to a number of government reports, less than 10 percent of the 80,000-odd chemicals in general commerce have been tested adequately to determine their health risks.
The U.S. Environmental Protection Agency recently announced the establishment of three new centers to develop alternative approaches for toxicity testing that could help fill the troubling gap. One is the Vanderbilt-Pittsburgh Resource for Predictive Toxicology (VPROMPT), which will receive $6 million for 4 years to develop toxicity test procedures based on 3-D human cell cultures, rather than the combination of standard 2-D cell cultures and whole animal testing that has been de rigueur until now.
VPROMPT is a collaboration between investigators at Vanderbilt University and the University of Pittsburgh. The center’s lead principal investigator is M. Shane Hutson, PhD, associate professor of physics at Vanderbilt. The five co-principal investigators are research associate professor Lisa McCawley, PhD, professor Kevin Osteen, PhD, director of the Women’s Reproductive Health Research Center, and Gordon A. Cain university professor John Wikswo, PhD, at Vanderbilt, and McGowan Institute for Regenerative Medicine associate director Rocky Tuan, PhD, director of the Center for Cellular and Molecular Engineering, and D. Lansing Taylor, PhD, director of the Drug Discovery Institute, both at Pittsburgh.
“Given the situation we face, traditional toxicology testing procedures are simply inadequate,” said Dr. Hutson. “A full toxicological evaluation for a single chemical using traditional methods can cost millions of dollars, involve hundreds of test animals, and take years to complete. And, as if the time and cost weren’t bad enough, existing tests haven’t proven very good at predicting chemicals’ effects on humans.”
The primary goal of the new center is to develop a series of 3-D human cell cultures that are heavily wired up with different sensors to record how they respond when exposed to small concentrations of potentially toxic chemicals. The forefront of cell biology is moving away from traditional 2-D culture of a single cell type towards 3-D cell culture of multiple cell types that more closely mimic the microenvironment of particular organs. These more complex cultures exhibit cell behaviors that are much more like those seen by cells in living animals. By making sure the cultures use human cells, the researchers hope to avoid misleading toxicity results caused by differences in how animal and human cells respond to the same chemical.
“We are very excited about the new Vanderbilt/Pittsburgh partnership to develop and apply innovative tissue-on-a-chip technologies to identify and evaluate potential harmful agents in the environment, and contribute towards improving the nation’s health,” said Dr. Tuan.
The researchers will develop four test platforms: one using liver cells; one using fetal membrane cells; one using mammary gland cells; and one using cells involved in limb and joint growth. They selected the liver because one of its functions is to remove toxic substances from blood coming from the digestive system before they can spread throughout the body. The fetal membrane and mammary gland cells were included because of the roles they play in reproduction. And they choose the cells involved in limb and joint growth because their role in development.
The researchers will expose the 3-D cultures to a battery of previously identified toxic chemicals that have been extensively studied using traditional methods so they can compare the results and determine how well the procedures they have developed predict the results of the older tests.
A Strategy for Stimulating Heart Muscle Regeneration in Infants, Study Finds
 Surgery often is life-saving for many infants born with heart defects, but one thing that doctors cannot do yet is replace heart muscle that is scarred and dysfunctional. McGowan Institute for Regenerative Medicine affiliated faculty member Bernhard Kühn, MD, director of research for the Division of Cardiology at Children’s Hospital, and associate professor of pediatrics at the University of Pittsburgh School of Medicine, and researchers from the Heart Institute at Children’s Hospital and Boston Children’s Hospital hope to overcome the challenge by stimulating regeneration of heart tissue. The findings were described in Science Translational Medicine.
Surgery often is life-saving for many infants born with heart defects, but one thing that doctors cannot do yet is replace heart muscle that is scarred and dysfunctional. McGowan Institute for Regenerative Medicine affiliated faculty member Bernhard Kühn, MD, director of research for the Division of Cardiology at Children’s Hospital, and associate professor of pediatrics at the University of Pittsburgh School of Medicine, and researchers from the Heart Institute at Children’s Hospital and Boston Children’s Hospital hope to overcome the challenge by stimulating regeneration of heart tissue. The findings were described in Science Translational Medicine.
Children born with congenital heart disease are at greater risk of developing heart failure even after surgical correction of the problem.
“It is not surprising that survivors often develop heart failure later on,” said lead author, Dr. Kühn. “But when these patients were given adult medicines in clinical trials, it turned out that they were not effective. The need for pediatric-specific heart failure therapies is increasingly recognized.”
For the study, the research team examined the potential of recombinant growth factor neuregulin-1 (rNRG1), which stimulates heart regeneration by driving proliferation of heart muscle cells, called cardiomyocytes.
They treated newborn mice with injections of rNRG1 at various times after heart injury and found that early treatment starting the first day after birth boosted cardiomyocyte cell division and heart function, and reduced scarring to a significantly greater degree compared to treatment that began at 5 days after birth. The growth factor also drove cardiomyocyte proliferation in lab tests of heart muscle samples obtained during surgery from human infants with congenital heart disease.
“These findings suggest that rNRG1 administration in infants with these birth defects might be a new therapeutic strategy for pediatric heart disease,” Dr. Kühn said. “Delivering agents early on that encourage the heart to make new cardiomyocytes could help the heart perform normally and reduce the risk of developing heart failure later in life.”
More research needs to be done before clinical testing of this strategy, the research team says. Dr. Kühn began the research while a member of the faculty at Boston Children’s Hospital.
AWARDS AND RECOGNITIONS
Badylak Lab Student Receives NSF Fellowship
 Jenna Dziki is a doctoral student within the Bioengineering Department at the University of Pittsburgh with research projects in the McGowan Institute of Regenerative Medicine laboratory of Stephen Badylak, DVM, PhD, MD. Based on Ms. Dziki’s recent grant proposal, “Extracellular Matrix Mediated Remodeling for Ulcerative Colitis Treatment,” she is the recipient of a fellowship under the 2015 National Science Foundation (NSF) Graduate Research Fellowship Program (GRFP).
Jenna Dziki is a doctoral student within the Bioengineering Department at the University of Pittsburgh with research projects in the McGowan Institute of Regenerative Medicine laboratory of Stephen Badylak, DVM, PhD, MD. Based on Ms. Dziki’s recent grant proposal, “Extracellular Matrix Mediated Remodeling for Ulcerative Colitis Treatment,” she is the recipient of a fellowship under the 2015 National Science Foundation (NSF) Graduate Research Fellowship Program (GRFP).
Her project proposal identifies inflammatory bowel disease (IBD) as an emerging global health problem, affecting an estimated 4 million people worldwide with increasing incidence. Ulcerative colitis (UC), one form of IBD, is characterized by diffuse, chronic inflammation of the gastrointestinal tract that confers not only a poor quality of life but it is also a risk factor for colorectal cancer. Recent advances in the understanding of UC etiology have spurred the development of new therapeutic strategies, however these remain pharmacological (e.g. steroids, immunosuppressives) or surgical (e.g. procolectomy) in nature and are associated with nonspecific systemic effects and toxicity, high recurrence and morbidity, and remain ineffective for severe, exacerbated cases of the disease.
Ms. Dziki’s work will determine whether diseased colonic mucosa can be successfully remodeled into healthy new mucosa using a regenerative medicine approach, a question that is central to improvement of therapy in UC as remodeling of diseased tissue into healthy new tissue aims to cure, not induce remission. In contrast to current surgical intervention, a regenerative medicine approach would be non-invasive and would result in colon preservation. Such significant potential of broader impact—to eliminate surgery as the standard of care of treatment of UC—warrants investigation. The results of her proposed work will lead to improved treatment strategies for UC, a disease affecting millions.
Overall, Ms. Dziki’s research focuses on the characterization of extracellular matrix (ECM)-mediated host innate immunomodulation and stem/progenitor cell activation. Specifically, Ms. Dziki is interested in macrophage polarization following ECM treatment in skeletal muscle and gut repair applications and the effects of polarized macrophages upon endogenous stem cell populations.
Congratulations, Ms. Dziki!
Woo Laboratory Students Claim Awards at International Symposium
 Two bioengineering graduate students under the mentorship of McGowan Institute for Regenerative Medicine faculty member Savio Woo, PhD, DSc, DEng, at the Musculoskeletal Research Center were the recipients of the Best Student Paper Award and Best Poster Award at the International Symposium on Ligaments and Tendons – XIV (ISL&T-XIV), which was held at the MGM Grand Hotel in Las Vegas, NV, on March 27, 2015.
Two bioengineering graduate students under the mentorship of McGowan Institute for Regenerative Medicine faculty member Savio Woo, PhD, DSc, DEng, at the Musculoskeletal Research Center were the recipients of the Best Student Paper Award and Best Poster Award at the International Symposium on Ligaments and Tendons – XIV (ISL&T-XIV), which was held at the MGM Grand Hotel in Las Vegas, NV, on March 27, 2015.
Ms. Katie Farraro (pictured left), her presentation entitled, “A Novel Magnesium Ring for Regeneration of an Injured Anterior Cruciate Ligament – In Vitro and In Vivo Studies in Goats,” was the recipient of the Best Student Paper Award.
Ms. Jonquil Flowers (pictured right), her presentation entitled, “A Novel Magnesium Based Suture Anchor for Soft Tissue Fixation,” was the recipient of the Best Poster Award.
Both presentations were selected by a panel of judges which included top notch investigators from all around the world in the field of ligament and tendon research.
Congratulations, Ms. Farraro and Ms. Flowers!
 Regenerative Medicine Podcast Update
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#146 – Dr. John Sinden is the Chief Scientific Officer at Reneuron, Inc. Dr. Sinden discusses his work developing novel stem cell therapies targeting areas of significant unmet or poorly met medical need.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
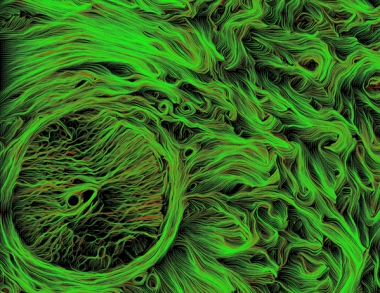
Picture of the Month
The Picture of the Month is a compliment to the longstanding features Grant of the Month and Publication of the Month. Each of these features highlights the achievements of McGowan affiliated faculty and their trainees. As we have always welcomed suggestions for grants and publications, please also consider submitting images that can highlight your pioneering work.
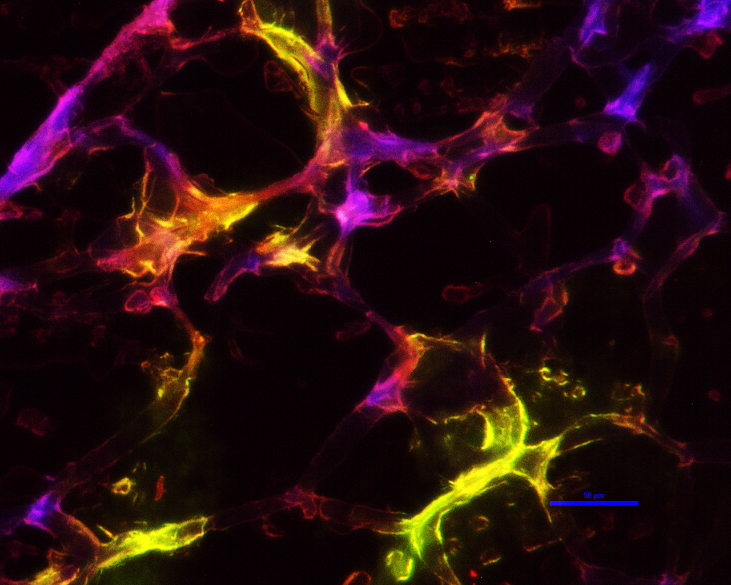
The image was taken using an inverted microscope and shows a co-culture of hMSCs and HUVECs. The staining on the image is for CD31 (red), a-sma (green), and nuclei (blue). The study is an in vitro investigation of sequential growth factor delivery for the formation of vascularized bone tissue.
Image provided by Emily Bayer. Mentors for this project are Dr. Steve Little (advisor) and Dr. Morgan Fedorchak.
