October 2021 | VOL. 20, NO. 10| www.McGowan.pitt.edu
Novel Gene Therapy Platform Speeds Search for Ways to Cure Blindness

A novel computational platform developed by researchers from the University of Pittsburgh School of Medicine identifies top-performing viral vectors that could deliver gene therapies to the retina with maximum efficiency and precision.
The technology, described in a paper published in the journal eLife, streamlines development of gene therapy approaches for the treatment of genetic blinding disorders. The approach saves precious time and resources by speeding up identification of suitable gene-carrying candidates able to deliver therapy to an affected part of the retina with astounding accuracy.
“Vision loss has a huge impact on quality of life. It has long been near the top of the greatest fears of people, alongside cancer and Alzheimer’s disease,” said senior author McGowan Institute for Regenerative Medicine affiliated faculty member Leah Byrne, PhD, Assistant Professor of Ophthalmology at Pitt. “But the field of vision restoration has entered a new era, where many patients have received effective treatment for the very first time. Because of that, the potential of our new platform is thrilling—it will allow us to translate emergent therapies that are already working for some patients into the clinic much more rapidly.”
McGowan Institute affiliated faculty member José-Alain Sahel, MD, Chair and Distinguished Professor of the Department of Ophthalmology at the University of Pittsburgh School of Medicine, director of the UPMC Eye Center, and the Eye and Ear Foundation Endowed Chair of Ophthalmology, is a co-author on the study.
Even though blinding genetic disorders that affect the retina are considered rare, approximately 1 in every 3,000 people worldwide carries one or more copies of broken genes that cause retinal degeneration and loss of vision. For centuries, many people with inherited blindness were all but guaranteed to spend a portion of their lives in darkness.
Now, with several gene therapies already on the market in Europe and the U.S., and dozens more entering clinical trials, hope for people with inherited blindness is within reach, but a key obstacle remains: ensuring that vectors, or inactivated viruses carrying the therapeutic genetic code, enter the exact cells that scientists are targeting. The retina is composed of hundreds of millions of cells that are arranged into a series of layers, so precisely targeting the vector to a specific location within that universe is not a trivial task.
To approach the problem, researchers developed a computational platform called scAAVengr, which uses single-cell RNA sequencing to evaluate quickly and quantitatively—among dozens of options—which adeno-associated virus vector, or AAV, is best suited for the task of delivering a gene therapy to a specific part of the retina.
The traditional approach of evaluating AAVs is painstakingly slow, requiring several years and many experimental animals. It also is not very precise since it doesn’t directly measure if AAVs not only entered the cells but also delivered their gene therapy cargo.
In contrast, scAAVengr uses single-cell RNA sequencing, which detects if the cargo arrives at its destination safely. And with scAAVengr, that process takes months, not years.
The platform’s uses aren’t just limited to the retina—the researchers showed that it works just as well for the identification of AAVs that target other tissues, including the brain, heart, and liver.
“A rising tide lifts all boats, and we hope that this technology propels gene therapy treatments not just in the field of vision restoration but for other purposes,” said Dr. Byrne. “Rapidly developing fields of gene editing and optogenetics all rely on efficient gene delivery, so the ability to quickly and strategically choose the delivery vectors would be an exciting leap forward.”
RESOURCES AT THE MCGOWAN INSTITUTE
November Histology Special – Herovici Staining
The Herovici combination of aniline blue or picro methyl blue and picro acid fuchsin results in Type I mature collagen staining red while reticulum and newly formed Type III collagen stains blue.
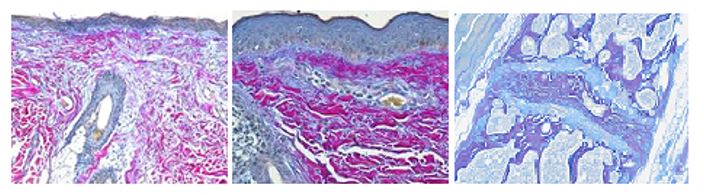
You’ll receive 25% off your Herovici staining in November when you mention this ad.
Contact Julia at the McGowan Core Histology Lab by email: Hartj5@upmc.edu or call 412-624-5265.
New Sample Submission Procedures: In response to COVID-19, we ask that you contact us to schedule a drop off time. When you arrive at the building you can call our laboratory at (412)624-5365. Someone will meet you in the lobby to collect your samples. When your samples are completed, you will receive an email to schedule a pickup time.
SCIENTIFIC ADVANCES
Development of Advanced Drug Delivery Systems to Address Global Environmental Challenge

On its face, agriculture seems simple: crops need water, sunlight, and soil to grow. The soil that crops are planted in, however, is complex. In order for plants to thrive, fertile soil requires a variety of elements that can become depleted over time, including nitrogen.
Nitrogen moves through the environment, changing forms as it goes from the atmosphere to the soil, to the plants rooted in the soil, to the animals that eat the plants, and finally back into the atmosphere. Agriculture can disrupt this loop—known as the nitrogen cycle—leading farmers to supplement more nitrogen into the soil, a practice with its own set of environmental risks.
An interdisciplinary team which brings expertise in chemical processes, transport phenomena, transport of natural resources in Earth systems, sustainable material design, and systems analyses is addressing this global challenge by developing technology that will more efficiently deliver nitrogen directly to crop roots, thereby preventing excess nitrogen from leaching into the environment. McGowan Institute for Regenerative Medicine faculty member Steven Little, PhD, Distinguished Professor and William Kepler Whiteford Endowed Professor and Chair of the Department of Chemical and Petroleum Engineering at Pitt, joins the project as co-principal investigator.
“It is exciting to work toward the development of advanced drug delivery systems where the ‘drug’ is a nutrient for crops,” said Dr. Little, whose expertise in such systems focuses on targeted treatment of medication at the site of injury or illness, rather than a diffused, large dose. “These kinds of delivery systems have been developed for years for pharmaceuticals, but less attention has been paid to this area. The potential for impact is pronounced since we’re talking about a similar problem. Why blanket an entire field of crops with nitrogen and risk runoff, when you can selectively deliver the nitrogen directly to the root?”
The research will be led by Leanne Gilbertson, PhD, associate professor of civil and environmental engineering at the University of Pittsburgh Swanson School of Engineering. The project recently received $1,699,999 from the National Science Foundation. Emily Elliott, PhD, Pitt professor of geology and environmental science and co-founder and director of the Pittsburgh Collaboratory for Water Research, Education, and Outreach, will also contribute.
“Rebalancing the nitrogen cycle is a global challenge,” said Dr. Gilbertson. “We were motivated to find a holistic, sustainable solution to feed society while protecting its prosperity.”
The overuse of nitrogen has immense environmental and human health costs, including the overgrowth of plant life in lakes and coastal waters that harm animal life; algal blooms and the dangers they pose; greenhouse gas emissions from the production of nitrogen-based fertilizer; on-farm greenhouse gas emissions from nitrogen processes; and contaminated drinking water.
To deliver nitrogen more directly, the researchers will study the use of liposomes – small spherical sacs containing nitrogen which serve as a delivery system that can increase the percentage of nitrogen absorbed by the plant. Farmers will need to use less nitrogen, diminishing the environmental risks.
“Excess nitrogen is one of the greatest threats to global ecosystem integrity and water quality,” said Dr. Elliott. “During my career as a biogeochemist, I’ve never been more excited to embark on a research project. If we are successful in building fertilizers that are retained in soils, this project will be a profound step forward in protecting ecosystems, water quality, and human health.”
“I am excited to work in an interdisciplinary team of researchers,” noted Dr. Gilbertson. “We are all experts in our respective areas and adept at thinking beyond our niches, across silos, and about big challenges. We will learn from each other over the next four years as we develop sustainable solutions to a global challenge.”
The project, “Sustainability from the Bottom Up: A Holistic Solution to Balancing the N-Cycle,” is a part of the NSF’s ECO-CBET program: Environmental Convergence Opportunities in Chemical, Bioengineering, Environmental, and Transport Systems. The program seeks to solve our most processing environmental and sustainability challenges with imaginative thinking from collaborating scientists across disparate fields.
COVID Antibody Tests: Are They Necessary?
McGowan Institute for Regenerative Medicine faculty member Alan Wells, MD, DMS, Thomas J. Gill III Professor of Pathology and the Executive Vice-Chairman of the Department of Pathology at the University of Pittsburgh, recently spoke with Michael Ollove, Staff Writer, Stateline, an initiative of The Pew Charitable Trusts, about COVID antibody tests. Talk of the need for COVID-19 booster shots has prompted many Americans to seek these tests.
In most cases, however, getting an antibody test to determine immunity is a fool’s errand, infectious disease doctors agree. The tests for antibodies, also known as serology tests, do not provide the answers that most people are seeking.
Both the federal Centers for Disease Control and Prevention and the Food and Drug Administration advise against using antibody tests to determine one’s level of immunity against COVID-19. So does the Infectious Disease Society of America, which represents infectious disease specialists.
While some states, including Maryland and South Carolina, are conducting targeted antibody testing for specific purposes, no state is promoting the tests’ use for residents to determine whether they have sufficient immunity or need a booster shot.
The tests might indicate the presence or even the level of COVID-19-fighting antibodies in the bloodstream, but scientists don’t yet know what number of antibodies provide protection from COVID-19. Antibodies are protein molecules the immune system produces to neutralize viruses or bacteria that have entered the body.
Antibody levels do help health care providers establish whether a patient has immunity against other, more familiar infectious diseases, such as measles and hepatitis A and B. But doctors say our relatively short experience with COVID-19 hasn’t yet provided the same information.
Testing for COVID-19 antibodies has some benefits—especially for determining whether someone with COVID-like symptoms had an earlier, undetected COVID-19 infection—but not for the reasons many are seeking the tests.
“Doctors are ordering antibody tests for people who are worried about waning immunity, but I see that as problematic,” said Dr. Wells, director of clinical labs at UPMC. “For a normal person, knowing your level eight months later [after their initial vaccine dosages] is of relatively little value.”
In general, the more antibodies, the better, Dr. Wells said. But even with a low level of antibodies months after exposure or receiving a vaccine, the body can mount a stout defense against the virus by generating new antibodies in response to a fresh infection. “There is more to your immune response than antibody levels,” said Dr. Wells.
Dr. Wells said the UPMC hospital, like others, has had a big increase in requests for antibody tests in recent weeks, though he recommends to his colleagues that they use them judiciously.
Another problem with COVID-19 antibody tests, doctors say, is that they are not standardized, so values associated with antibody tests in one version might not be the same as another.
Without knowing what level of antibodies provides immunity or the parameters—especially the timing—of testing vaccinated people, such a measure may not provide the assurance its sponsors suggested. But Dr. Wells added that the idea is not without merit, because higher levels of antibodies do correlate with fewer hospitalizations and deaths.
Using AI to Treat Acute Kidney Injuries

Among critically ill patients with acute kidney injury and treated with dialysis in the intensive care unit, if one could accurately predict early which patients will develop low blood pressure then effective treatments could be given. In a recently funded study, co-principal investigators McGowan Institute for Regenerative Medicine affiliated faculty member Gilles Clermont, MD, Professor of Critical Care Medicine at the University of Pittsburgh, and Raghavan Murugan, MD, Professor of Critical Care Medicine at Pitt, and their team propose to develop and validate an artificial intelligence system that will predict low blood pressure even before it occurs and recommend correct treatment to clinicians. McGowan Institute affiliated faculty member Robert Parker, PhD, Professor in the Department of Chemical and Petroleum Engineering at Pitt, is a member of this team that will receive funding for an NIH grant proposal entitled “AI driven acute renal replacement therapy (AID-ART).” The award is for $2.9M and is for 4 years from the National Institute of Diabetes and Digestive and Kidney Diseases.
The abstract for the project follows:
Intradialytic hypotension (IDH) occurs in one-third of critically ill patients with acute kidney injury and treated with kidney replacement therapy in the intensive care unit (ICU). Occurrence of IDH is associated with increased resource utilization such as fluid and vasopressor administration, discontinuation of kidney replacement therapy, decreased recovery of kidney function, dependence on kidney replacement therapy, and death. IDH is often unrecognized until it is well established, by which time patients are refractory to treatment or have already developed organ injury. Thus, if one could accurately predict who and when patients develop IDH, then effective preemptive treatments could be administered to reduce risk of IDH and improve outcomes. Our preliminary work showed that advanced high-frequency data modeling and waveform analysis identified patients at risk for hypotension within 2 minutes of monitoring in the ICU, and if monitored for 5 minutes, differentiated between patients who would develop hypotension or remain stable over the next 48 hours. In this proposal entitled “Artificial Intelligence Driven Acute Renal Replacement Therapy (AID-ART),” we propose to apply predictive analytics using linked electronic health record and high-frequency monitor data to critically ill patients with acute kidney injury and undergoing intermittent and continuous kidney replacement therapies at the University of Pittsburgh Medical Center and the Mayo Clinic ICUs. We will examine the accuracy of various machine learning models to predict IDH risk-evaluating model performance, usability, alert frequency, lead time, and number needed to alert, and hospital mortality and dependence on kidney replacement therapy (Aim 1a); predict response to a range of clinical interventions for IDH and subsequent clinical outcomes (Aim 1b); and perform cross validation across the two healthcare systems (Aim 1c). We will construct reinforcement learning systems to develop a rule-driven intervention for IDH alerts and measurement-driven responses to avoid and respond to IDH based on principles of functional hemodynamic monitoring (Aim 2a). We will also develop a reinforcement learning algorithm to learn an optimal intervention strategy based on the probability of events rather than in reaction to IDH events (Aim 2b). We will silently deploy and evaluate the ability of this artificial intelligence (AI) algorithm to forecast IDH risk and recommend interventions in real-time across the two healthcare systems. We will then assess the validity of recommended interventions using an expert clinician adjudication panel (Aim 3a); and will compare the AI recommended interventions with that of actual interventions performed by bedside clinicians (Aim 3b). This proposal will be the harbinger of a future multicenter randomized clinical trial to examine personalized risk prediction and AI-augmented management of IDH among critically ill patients with acute kidney injury and undergoing kidney replacement therapy in the intensive care unit.
Illustration: Department of Critical Care Medicine, University of Pittsburgh (Gilles/Murugan) and Department Chemical and Petroleum Engineering (Parker)
Identification of Therapeutic Strategies to Prevent or Halt Progression of Chronic Liver Diseases

There is growing evidence that cellular senescence plays a critical role in the pathogenesis of chronic liver diseases. McGowan Institute for Regenerative Medicine affiliated faculty member Michael Oertel, PhD, Associate Professor of Pathology, Division of Experimental Pathology, Department of Pathology, and a member of the Liver Research Center at the University of Pittsburgh, is a co-principal investigator on a project that will dissect the role of the activin A/p15INK4b axis in inducing senescence and how it impacts chronic liver disease progression. Uncovering mechanism(s) and identifying essential mediators of hepatocyte senescence will provide fundamental new information for developing novel therapeutic strategies to halt progression of chronic liver diseases.
The project is entitled, “Blocking Hepatocyte Senescence as a Novel Therapeutic Strategy for Chronic Liver Diseases,” will run for 4 years. The National Institute of Diabetes and Digestive and Kidney Diseases of the NIH funded this project.
The abstract of the project follows:
There is growing evidence implicating that cellular senescence is involved in the progression of chronic liver diseases (CLD). However, the mechanisms underpinning cellular senescence-mediated progression of CLD remain unclear. We have recently reported an important role of the activin A/p15INK4b axis in inducing hepatocyte (HC) senescence. Further suggesting a role of the activin A/p15INK4b axis in inducing HC senescence in CLD, because our preliminary data from rat models of liver cirrhosis revealed increased activin A and p15INK4b expression in cirrhotic liver tissue regions, which correlated with increased hepatic SA-β-gal activity. We also found that elevated p15INK4b expression in the livers of mice treated with CCl4 and observed that activin A inhibition markedly reduced CCl4-induced hepatic injury. Increased levels of activin A are also reported in several human CLDs, and our preliminary data demonstrate increased activin A expression in the livers of cirrhosis patients. Based on this evidence, we hypothesized that activin A contributes to the pathogenesis of CLDs by driving p15INK4b-mediated induction of HC senescence. Senescence-associated secretory phenotype (SASP) factors produced by senescent HCs promote inflammation and fibrosis, resulting in CLD progression. We will test our hypothesis using our established rat HC transplantation model and rodent models of CLD according to the following integrated Specific Aims. In Aim 1, we will use our HC-transplantation model to precisely demarcate senescent and neighboring cells, followed by isolation of both cell populations using laser-capture microdissection (LCM). Comparative analyses of these foci and their surrounding regions will reveal paracrine signals from senescent HCs and their phenotypic effects on neighboring HCs. Aim 2 will investigate the effect of activin A/p15INK4b-induced HC senescence in both rat and mouse models of CLD. Studies in the mouse model will also include a comprehensive phenotypic and functional analysis of hepatic immune cell infiltrates to determine the impact of HC senescence on immune cells. We will also evaluate hepatic expression of activin A and p15INK4b in cirrhotic patients by confocal microscopy to determine the clinical relevance of the activin A/p15INK4b axis. Lastly, in Aim 3, we will investigate the therapeutic benefit of targeting senescence in CLDs. This application leverages our combined expertise in liver transplantation models (Oertel, MPI), animal models of liver diseases (Oertel/Raeman, MPIs), immunology (Raeman), and senescence (Oertel), as well as extensive experience in hepato-pathology and RNA-seq analyses (Locker, Co-I) and lentiviral/AAV expression systems (Bell, Co-I), to investigate the mechanisms underpinning HC senescence and the role of senescent HCs and their detrimental effects on neighboring cells in the pathogenesis of CLD. The results of our investigations will lead to identification of therapeutic strategies to prevent or halt progression of CLD by targeting hepatic senescence.
Convalescent Plasma Futile as Treatment for Critically Ill COVID-19 Patients

In the earliest days of the COVID-19 pandemic, the medical community turned to a century-old treatment: Take blood from recovered patients and give it to the sick. The hypothesis was that components in the so-called “convalescent plasma” that fought off the disease once could do it again, something that has worked in other diseases, such as Ebola.
Today, an international research team, which included University of Pittsburgh School of Medicine physician-scientists and UPMC patients, effectively put an end to that practice with a clinical trial that concluded convalescent plasma is “futile” as a COVID-19 treatment for most critically ill patients. The results are published in JAMA concurrent with presentation at the European Society of Intensive Care Medicine’s annual meeting. McGowan Institute for Regenerative Medicine affiliated faculty member Derek Angus, MD, MPH, chief innovation officer at UPMC and chair of the Department of Critical Care Medicine at Pitt, is a co-senior author of the study.
“There were biologically plausible reasons to turn to convalescent plasma early in the pandemic when hundreds of thousands of people were getting sick and treatments had yet to be discovered,” said co-lead author Bryan McVerry, MD, associate professor of pulmonary, allergy and critical care medicine at Pitt and a UPMC intensivist. “Unfortunately, it was either being administered outside of clinical trials or in trials that weren’t focused on critically ill patients, slowing our ability to see if it actually worked. Finally, with these results, we can put an end to using convalescent plasma for our sickest COVID-19 patients and focus on treatments that we know work, as well as developing and testing better ones.”
The findings are the latest from REMAP-CAP (Randomized, Embedded, Multifactorial, Adaptive Platform Trial for Community-Acquired Pneumonia), which has enrolled thousands of patients in hundreds of hospitals around the world to quickly determine what COVID-19 treatments work best in which patients. To date, more than 400 UPMC patients have been enrolled. Among its discoveries, REMAP-CAP has shown that inexpensive steroids are effective in helping critically ill patients, while blood thinners help the moderately ill.
In the convalescent plasma trial, REMAP-CAP enrolled 2,011 adults hospitalized with severe COVID-19. They were randomized to either receive two units of convalescent plasma or no plasma and followed to see if the likelihood of surviving at least three weeks without needing organ support, such as a ventilator, differed based on whether they were treated or not.
The trial concluded for futility when enough data was collected to say with greater than 99% certainty that convalescent plasma did not help critically ill COVID-19 patients.
However, the results followed a slightly different pattern for the 126 patients who were immunocompromised. This group appeared to do slightly better with the convalescent plasma treatment compared to the standard treatment, but the number of patients was too small to make a definitive statement.
“It could be that patients with an impaired immune system, who are unable to mount an effective immune response, could still benefit from the antibodies present in blood plasma from COVID-recovered patients, especially early on in the illness,” said corresponding author Lise Estcourt, M.D., an associate professor of hematology and transfusion medicine at the Oxford University’s Radcliffe Department of Medicine and director of the U.K.’s National Health Service Blood and Transplant Clinical Trials Unit. “This is something that definitely warrants investigation.”
The researchers could not determine why convalescent plasma did not improve outcomes in most critically ill patients.
“We speculate that it could be a combination of too few high-quality antibodies in the plasma and these patients being too far along in their illness with a run-away inflammatory immune response for those antibodies to turn the tide,” said Dr. Angus. “It is still possible that convalescent plasma helps people in earlier stages of illness, though it is likely not efficient to use given that monoclonal antibodies—which UPMC also is evaluating in our OPTIMISE-C19 adaptive trial—are such an effective treatment for early COVID-19.”
Additional co-authors of this research from Pitt or UPMC are David T. Huang, MD, MPH, Kelsey Linstrum, MS, Stephanie Montgomery, MSc, Christopher Seymour, MD, MSc, John McDyer, MD, and Darrell Triulzi, MD. Authors at other institutions are listed in the JAMA manuscript.
This research was supported by the UPMC Learning While Doing Program, as well as multiple other funders listed in the JAMA manuscript.
Illustration: McGowan Institute for Regenerative Medicine.
Like Priming a Pump, Changes in Cells Damaged by Chronic Lung Disease Can Result in Severe COVID-19

The results of a study by an international scientific team co-led by the Translational Genomics Research Institute (TGen), an affiliate of City of Hope, suggest that — like pouring water atop a wellhead before pumping — the airway cells of patients with chronic lung diseases are “primed” for infection by the COVID-19 virus, resulting in more severe symptoms, poorer outcomes, and a greater likelihood of death.
The study — published in Nature Communications — details the genetic changes caused by chronic lung disease in the molecular makeup of a variety of cells, including the epithelial cells that line the lung and airways. The study details how those changes can help enable SARS-CoV-2, the virus that causes COVID-19, to enter the body, replicate and trigger an out-of-control immune response that fills the lungs with fluids and often results in patients needing respirators and lengthy hospitalizations.
The team used single-cell RNA sequencing technology to spell out the genetic code of 611,398 cells from various data bases, representing those with both healthy (control) lungs and those with chronic lung disease. Sequencing and analysis allowed researchers to identify molecular characteristics that may account for worse COVID-19 outcomes.
“Our results suggest that patients with chronic lung disease are molecularly primed to be more susceptible to infection by SARS-CoV-2,” said Nicholas Banovich, PhD, an Associate Professor in TGen’s Integrated Cancer Genomics Division, and one of the study’s senior authors. Dr. Banovich is a leading participant in the Human Cell Atlas Lung Biological Network, whose dozens of members — including McGowan Institute for Regenerative Medicine affiliated faculty member Mauricio Rojas, MD, Professor of Internal Medicine and the Associate Vice Chair of Research, Department of Internal Medicine, in the Division of Pulmonary, Critical Care, & Sleep Medicine of the Davis Heart & Lung Research Institute at The Ohio State University — representing more than 80 institutions worldwide, also contributed to this study.
In addition, older-age, male-gender, smoking, and co-morbidities such as high blood pressure, obesity and diabetes, are all COVID-19 risk factors that are exacerbated by chronic lung diseases, such as Chronic Obstructive Pulmonary Disease (COPD), Interstitial Lung Disease (ILD), and especially Idiopathic Pulmonary Fibrosis (IPF), a progressive scaring and stiffening of the lung tissue.
“It was recognized early in the pandemic that patients with chronic lung diseases were at particularly high risk for severe COVID-19, and our goal was to gain insight into the cellular and molecular changes responsible for this,” said Jonathan Kropski, MD, Associate Professor of Medicine and Cell and Developmental Biology at Vanderbilt University Medical Center, and a co-senior author of the study.
Changes in lung cells and immune cells
Researchers specifically searched for changes in AT2 cells, a major lung epithelial cell type, focusing on cellular pathways and expression levels of genes associated with COVID-19. They established a “viral entry score,” a composite of all genes associated with SARS-CoV-2 and found higher scores among cells from patients with chronic lung disease.
They also explored changes in immune cells and discovered dysregulated gene expression associated with hyper-inflammation and with sustained cytokine production, two signature symptoms of severe SARS-CoV-2 infection. So-called cytokine storms in COVID-19 patients unleash a cascade of immune cells that flood the lungs, causing severe organ damage.
“The genetic changes in immune cells, especially in specialized white blood cells known as T cells, may diminish the patient’s immune response to viral infection and lead to higher risk of severe disease and poor outcomes in patients with chronic lung disease,” said Linh Bui, PhD, a post-doctoral fellow in Dr. Banovich’s lab, and one of the study’s lead authors.
“Our data suggest that the immune microenvironment at both the molecular and cellular levels in lungs damaged by chronic diseases may promote severe COVID-19,” Dr. Bui said.
Pneumococcal Extracellular Vesicles Modulate the Immune Response

Small vesicles secreted by bacterial cells play a role in recruiting immune cells but surprisingly also might help to protect the pathogens, according to a new study from Carnegie Mellon University and University of Pittsburgh researchers published in mBio. The study is one of the first studies to look at the role of extracellular vesicles released by the pathogen pneumococcus in vivo and may provide a new avenue for vaccine development.
Extracellular vesicles (EVs) are small packages that are released from almost all types of cells. Inside the packages can be a variety of cellular material, including proteins and nucleic acids. The vesicles travel between cells to deliver their cargo.
“Extracellular vesicles are the universal communicators across all living cellular organisms. They allow cross-communication between kingdoms,” said Phil Campbell, PhD, a professor of biomedical engineering at Carnegie Mellon University and a McGowan Institute for Regenerative Medicine affiliated faculty member.
These vesicles have become of particular interest for their potential to diagnose or treat disease; they are promising vaccine candidates, as they come from and carry information from pathogenic cells but cannot replicate. Most research on EVs has been done on cells from eukaryotic multicellular organisms, like humans, and not on prokaryotic single-celled organisms like bacteria, especially bacteria with a thick cell wall like pneumococcus.
“The wonderful thing about extracellular vesicles is that they express a huge amount of molecules from the pathogen,” said N. Luisa Hiller, PhD, associate professor of biological sciences at Carnegie Mellon. “If you think about them in the context of vaccines, you could provide the body with the opportunity to mount defenses against a large subset of molecules from the pathogen. But since the vesicle isn’t a pathogen itself, it won’t make you sick in the same way the bacteria make you sick.” This strategy of using multiple molecules in a vaccine could be a powerful means of ensuring that the vaccine is still effective, even if the pathogen mutates.
To get a better understanding of bacterial EVs, Dr. Hiller, whose research focuses on cellular communication in the pathogen Streptococcus pneumoniae, commonly called pneumococcus, teamed up with Dr. Campbell, an expert in extracellular vesicle research.
In their study, the interdisciplinary research team led by biomedical engineering graduate student Saigopalakrishna S. Yerneni isolated EVs from pneumococcus and studied their interaction with other cells both in vitro and in vivo. In vitro, they found that the bacterial EVs were internalized by macrophages, T cells and epithelial cells — all cells that play a role in the immune response.
Most importantly, they found that exposure to pneumococcal EVs caused human macrophages to polarize into the immunosuppressive, anti-inflammatory M2 phenotype, which are not well suited to kill bacteria. Exposure to EVs conditioned the macrophages to increase their bacterial uptake, possibly creating a reservoir for the bacteria.
In mouse models, the research team found that the EVs induced cytokine release and recruited lymphocytes and macrophages, all important components of the immune response. Moreover, they found an abundance of anti-inflammatory macrophages, agreeing with the data from the in vitro studies.
Overall, the data show that the pneumococcal EVs can be internalized into host cells and promote the cells’ defenses by recruiting inflammatory cells. But they also promote bacterial survival by creating an anti-inflammatory environment.
“The EVs recruited immune cells, which is an advantage for the host cells. But the type of macrophages that were recruited provided an advantage for the bacteria by creating a place where the bacteria may be able to hide and survive,” said Dr. Hiller. “It seems that things have evolved to provide advantages to both the host and the bacteria in a type of arms race.”
One of the next steps in the research is to determine how bacterial EVs could be used as therapeutics and vaccines. This is especially relevant as the World Health Organization estimates that close to a half a million children under the age of five die from pneumococcal disease every year and current vaccines do not provide protection against all strains. EVs may prove to be a valuable tool to develop a broad-spectrum vaccine that targets all strains.
Illustration: Carnegie Mellon University.
Dopamine Fasting: Is It Possible?

Often inaccurately hyped up as the “pleasure molecule,” dopamine is implicated more in “pursuing” than producing pleasure, explains Rabeea Saleem in her article for The National. For example, if you enjoy a sugar rush, dopamine is responsible for motivating you to seek a cupcake to satisfy your cravings, rather than the actual rush. She spoke with McGowan Institute for Regenerative Medicine affiliated faculty member Zachary Freyberg, MD, PhD, assistant professor in the Departments of Psychiatry and Cell Biology at the University of Pittsburgh, for her article.
Dopamine acts as a key motivator in maintaining addictive behavior, which is why the level of dopamine released can be used to gauge the addictiveness of a particular object or experience.
Dopamine also plays a key role in our motivation, pleasure, and reward system. It boosts mood and attention while helping to regulate our movement, learning, sex drive, and emotional responses. Meanwhile, imbalance of dopamine levels plays a significant part in a host of mental health problems, including psychiatric illnesses such as schizophrenia, bipolar disorder, and Parkinson’s disease.
Meanwhile, dopamine fasting has been popularized by wellness influencers. It is the antidote to overstimulation and consists of abstention from food, drugs, and other desires, and in some extreme cases, talking to other people for 24 hours or more. In many ways it is the rebranding of the traditional fasting practiced for religion and older wellness fads such as intermittent fasting.
The end goal is a brain “reset” for a decluttered, more focused brain. But this moniker is misleading because complete dopamine abstinence is not possible.
“Dopamine fasting is a prime example of exaggerating the role of dopamine,” says Dr. Freyberg, who studies human disorders of dopaminergic neurotransmission, including addiction, schizophrenia, and Parkinson’s disease.
“In itself, this is good as it makes people more mindful of their surroundings and of themselves as they take a pause from screens.”
But the idea of fasting from dopamine is misleading because it does not actually deplete the chemical or block its activity in the brain, because it is also used for a variety of other functions.
“For example, dopamine is essential for coordinating basic movement, and when its levels drop in the brain, this can create movement difficulties,” Dr. Freyberg says.
A more accurate description would be a stimulation fast or unplugging from the world. Dopamine acts as a “switchboard” that tunes and helps direct our attention and budget our energy levels. Our brain is more than the sum of its parts, so a holistic approach is more useful in understanding how it interacts with our behavior.
BRAIN Initiative Funding Received for BCI Development and Testing

A person suffering from amyotrophic lateral sclerosis (ALS) endures the progressive loss of muscle function throughout their body. Eventually, they lose the ability to control their limbs, to swallow, and even to speak. Their inability to communicate becomes a particularly devastating symptom of the illness. Other diseases can cause similar, debilitating impairment.
Restoring functionality and well-being to these individuals requires an innovative and collaborative approach.
Carnegie Mellon University is leading a multidisciplinary consortium of researchers to develop and test a minimally invasive, brain-computer interface (BCI) in six patients with severe paralysis from ALS, stroke, and injury, among other causes. The system will enable these patients to operate computers and send digital communications, such as email and text messaging, by sensing and interpreting signals in the brain that express the user’s intent. McGowan Institute for Regenerative Medicine affiliated faculty member Doug Weber, PhD, professor of mechanical engineering and neuroscience at Carnegie Mellon University, is leading the collaboration.
The $9.33M project, funded by the National Institutes of Health (NIH) Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative, will evaluate the BCI’s safety and efficacy in providing a measurable improvement in independence and quality of life. Collaborators include Mount Sinai Health System (New York), Synchron, Inc. (New York), and the University of Pittsburgh Medical Center (Pennsylvania). The team combines expertise in engineering, medicine, neuroscience, and biomedical device technology.
The BCI, called the StentrodeTM, is the only BCI system that can be implanted in the brain without opening the skull or penetrating brain tissue. Instead, it is implanted through blood vessels that provide a natural and safe passageway for accessing the motor cortex, the portion of the brain that controls movement in the body. It is being commercialized by the company Synchron, Inc.
Carnegie Mellon researchers bring additional expertise in brain-computer interface to the project. They will explore machine learning methods for processing and decoding brain signals to detect the user’s intended actions and a haptic feedback interface for improving speed and accuracy of BCI control.
“The human body is an amazing machine, but it cannot heal itself from many diseases and injuries. This is where combining multidisciplinary expertise with emerging new technologies can make a significant impact,” said Dr. Weber. “Our team of engineers and neuroscientists will be working together with Synchron to evaluate and enhance capabilities of its BCI for restoring functionality in patients in this study and for future BCI applications.”
Detecting brain signals with a sensor placed inside a blood vessel represents an emerging new sub-discipline of medicine. “By using the blood vessels as the natural highway into the brain, we can access all areas, which traditionally required open surgery and removal of skull in multiple areas,” said Thomas Oxley, MD, PhD, chief executive officer, Synchron.
The system detects electrical signals generated by neurons in the motor cortex when the person thinks about moving their body, and these signals are transmitted wirelessly to an external interface connected to a computer. Users will be trained to perform computer-based tasks to control cursor position and BCI outputs to control discrete actions, such as letter or menu-item selection and zoom.
The technology will facilitate better communication between patients, caregivers, and medical professionals. In addition, it will empower these patients to experience functional independence in performing daily tasks like online shopping and banking.
“This technology has the potential to revolutionize our ability to care for patients by solving health challenges that have previously been insurmountable including communication with patients with certain types of paralysis,” said David Putrino, PhD, director of rehabilitation innovation for the Mount Sinai Health System (one of the sites involved in the trial) and associate professor of rehabilitation medicine at Icahn School of Medicine at Mount Sinai.
Another site, UPMC and the University of Pittsburgh’s Rehab Neural Engineering Labs (RNEL), will work together to recruit patients. RNEL—directed by McGowan Institute affiliated faculty member Michael Boninger, MD, professor in the Department of Physical Medicine & Rehabilitation at the University of Pittsburgh School of Medicine—will run tests and functional MRIs to determine which patients selected by a neuromuscular specialist and pulmonologist meet the entry criteria for implantation. A vascular neurologist will perform the BCI implantation surgery and physicians will monitor the subject’s clinical status.
BCIs have previously been limited to people involved in research studies, and only for the duration of their enrollment in the study. At the end of this trial, however, the six patients involved will retain use of the BCI technology. The aim is to make the technology broadly accessible.
In the future, those suffering from a range of medical conditions such as limb amputation, multiple sclerosis, and Parkinson’s disease might benefit from this research.
New Material Aids in Neural Stimulation

The ability to target and stimulate neurons brings a host of benefits including better understanding brain function and treating neurological diseases. Currently, state-of-the-art microelectrode arrays (MEAs) can stimulate neurons with high precision, but they lack cell-type specificity and require invasive implantation that can result in tissue damage—think stimulators used to help patients with tremors. McGowan Institute for Regenerative Medicine affiliated faculty member Tzahi Cohen-Karni, PhD, associate professor of materials science and engineering and biomedical engineering at Carnegie Mellon University, and his team have been exploring new materials to allow remote photostimulation, or the use of light to stimulate cells.
Cells can “talk” with one another by sending and receiving electrical signals. Inside a cell’s membrane, a neuron in our brain for example, there are tiny pores called ion channels that let ions move in and out of the cell. Under normal conditions, the fluxes of ions across the membrane dictate whether a cell will send an electrical signal to its neighbors. In recent years, researchers have shown that it is possible to use pulses of light to alter the cell membrane’s properties and elicit an electrical signal that can control cellular communication. Dr. Cohen-Karni’s team aims to identify materials effective at controlling cell activities without causing distress. They recognized that multi-dimensional graphene (fuzzy graphene) posed as a great candidate for cellular stimulation but found that some materials were difficult to produce and couldn’t absorb enough light to efficiently transfer light to heat.
In his current research published by the American Chemical Society, Dr. Cohen-Karni focused on transition metal carbides/nitrides (MXenes) flakes, a unique two-dimensional nanomaterial discovered by Yury Gogotsi’s team at Drexel University. MXenes have been demonstrated to exhibit outstanding mechanical properties, high electrical conductivity, and excellent electrochemical properties, and they are easy and inexpensive to produce.
Rather than study the material for its bulk properties, Dr. Cohen-Karni’s team measured the photothermal properties of the material at a single flake level. The team dispersed flakes on the surface of dorsal root ganglion (DRG), cells in the peripheral nervous system, and illuminated them with short pulses of light. By studying the interface between cells and materials it became clear that flakes would not be absorbed by the cells, and Dr. Cohen-Karni could accurately measure the amount of light required to create cellular change.
“What is really unique about the materials that we are using in my lab is that we don’t need to use high energy pulses in order to get an effective stimulation,” Dr. Cohen-Karni explained. “By shining short pulses of light on the DRG-MXene interface, we found that the electrophysiology of the cell was successfully altered.”
So, what does this mean for the future of neurology? With an increased understanding of how to achieve neural stimulation and the ease of MXene production, researchers can more efficiently practice remote photostimulation. For example, researchers could embed MXenes into artificial tissue engineered in the form of a brain, and then use light to control the neural activity and further uncover the role of neurons in brain development. Eventually, this material could even be used as a non-invasive treatment for neural function disabilities, like tremors.
Dynamic Heart Model Advances Engineered Heart Tissue Tech

Efforts to understand cardiac disease progression and develop therapeutic tissues that can repair the human heart are just a few areas of focus for the Carnegie Mellon University (CMU) research group of Adam Feinberg, PhD, a Professor of Biomedical Engineering and Materials Science and Engineering at CMU and an affiliated faculty member of the McGowan Institute for Regenerative Medicine at the University of Pittsburgh. The group’s latest dynamic model, created in partnership with collaborators in the Netherlands, mimics physiologic loads on engineering heart muscle tissues, yielding an unprecedented view of how genetics and mechanical forces contribute to heart muscle function.
“Our lab has been working for a long time on engineering and building human heart muscle tissue, so we can better track how disease manifests and also, create therapeutic tissues to one day repair and replace heart damage,” explains Dr. Feinberg. “One of the challenges is that we have to build these small pieces of heart muscle in a petri dish, and we’ve been doing that for many years. What we’ve realized is that these in-vitro systems do not accurately recreate the mechanical loading we see in the real heart due to blood pressure.”
Hemodynamic loads, or the preload (stretch on heart muscle during chamber filling) and afterload (when the heart muscle contracts), are important not only for healthy heart muscle function, but can also contribute to cardiac disease progression. Preload and afterload can lead to maladaptive changes in heart muscle, as is the case of hypertension, myocardial infarction, and cardiomyopathies.
In new research published in Science Translational Medicine, the group introduces a system comprised of engineered heart muscle tissue (EHT) that is attached to an elastic strip designed to mimic physiologic preloads and afterloads. This first-of-its-kind model shows that recreating exercise-like loading drives formation of more functional heart muscle that is better organized and generates more force each time it contracts. However, using cells from patients with certain types of heart disease, these same exercise-like loads can result in heart muscle dysfunction.
“One of the really important things about this work is that it’s a collaborative effort between our lab and collaborators in the Netherlands, including Cardiologist Peter van der Meer,” says Dr. Feinberg. “Peter treats patients that have genetically-linked cardiovascular disease, including a type called arrhythmogenic cardiomyopathy (ACM) that often becomes worse with exercise. We have been able to get patient-specific induced pluripotent stem cells, differentiate these into heart muscle cells, and then use these in our new EHT model to recreate ACM in a petri dish, so we can better understand it.”
Jacqueline Bliley, a biomedical engineering graduate student and co-first author of the published paper, adds, “The collaborative nature of this work is so important, to be able to ensure reproducibility of the research and compare findings across the world.”
Looking to the future, the collaborators aim to use their model and findings to study a wide range of other heart diseases with genetic mutations, develop new therapeutic treatments and test drugs to gauge their effectiveness.
“We can take lessons learned from building the EHT in a dish to create larger pieces of heart muscle that could be used therapeutically. By combining these new results with our previous work involving 3D bioprinting heart muscle (published in Science in 2019), we hope to one day engineer tissues large and functional enough to implant, and repair the human heart,” projects Dr. Feinberg.
Lightening the Load of Multi-Material Manufacturing with 3D Printing

The rise of 3D printing has transformed the manufacturing industry, enabling manufacturers to quickly, and precisely, create specialized parts for any application. Numerous applications are envisaged for this technology, ranging from flexible electronics, soft robotics, architected materials, and biological tissues.
3D printing has enabled the production of components made of multiple materials, each with their own unique properties. However, the process—which typically includes changing out vats of liquid and cleaning the lines in the middle of production—causes slow-downs and increases costs.
Research led by University of Pittsburgh engineers—including McGowan Institute for Regenerative Medicine affiliated faculty member Sachin Velankar, PhD, professor of chemical and petroleum engineering, University of Pittsburgh—promises to streamline this process by using different wavelengths of light to create reactions that imbue one specialized material system with different properties, rather than changing out the material itself to achieve the same goal. The research recently received $500,000 in funding from the National Science Foundation (NSF) Future Manufacturing Seed Grant.
“Existing multi-material manufacturing methods have to switch over the material in the middle of production, rotating between materials like resins and waxes to create a single component,” explained Xiayun Zhao, PhD, assistant professor of mechanical engineering and materials science at Pitt, who is leading the project. “Instead, we’re advancing the use of a single resin vat that can replace that process by exhibiting different characteristics when cured with different wavelengths of light.”
Unlike the popular, consumer 3D printers that melt a filament of solid material to print layers, the 3D printing that is used for manufacturing is more complex, using a liquid that is cured by light exposure using a laser as the layers are printed into place. Prior research has explored the use of wavelength selectivity to create distinct reactions that cure material for 3D printing in different ways. This project is the first systematic and comprehensive study to establish the chemistry theory in the practice of multi-material photopolymer 3D printing.
“It’s traditionally very hard, but very useful, to use multiple materials within a single, complex, 3D shape,” said Dr. Velankar, co-principal investigator. “3D printing has made it more attainable, but it’s still difficult. By using two lasers of different wavelengths, we can bypass the slowest part of the process.”
Joining Drs. Zhao and Velankar is Sarah Bergbreiter, PhD, professor of mechanical engineering at Carnegie Mellon University. Dr. Bergbreiter will apply the technology in her soft robotics and sensors work to test its capabilities.
“I’m particularly excited to explore the possibility of printing conductive materials and structural materials simultaneously for robotics applications,” said Dr. Bergbreiter.
The project, “Establishing a Cyber-Physical Framework and Pilot System of Wavelength Selective Photopolymerization Based Rapid Continuous Multi-Material Manufacturing,” begins Jan. 15, 2022, and will extend through 2023.
Magee-Womens Research Institute Announces Finalists for $1 Million Prize

Magee-Womens Research Institute (MWRI) will award the $1 million Magee Prize to an international team of scientists during the Magee-Womens Summit November 16 to 18, 2021. The prize will help fund new research initiatives and transdisciplinary collaborations to promote knowledge and enhance the health and wellness of women and infants worldwide.
Three Magee Prize finalist teams were selected, one of which includes McGowan Institute for Regenerative Medicine affiliated faculty team members. That project is:
Vaginal Stem Cells: The Missing Link in Vaginal Reconstruction
Pamela Moalli, MD, PhD (MWRI/University of Pittsburgh); Kyle Orwig, PhD (MWRI/University of Pittsburgh), Caroline Gargett, PhD. (Monash University, Australia)
An increasing number of women are seeking vaginal reconstruction surgery to repair tissue loss after surgery for pelvic cancers or following ovariectomy, chemotherapy and radiation, which can result in the vagina becoming contracted, thinned, and painful. After noticing the limited range of biomaterials for these procedures, Dr. Moalli was inspired to develop better solutions. This project seeks to identify stem cell populations that restore vaginal structure and function and isolate the cellular ecosystems needed for stem cell survival, proliferation, and engraftment. The researchers will use a novel bioassay to develop vaginal organoids from vaginal stem cells.
“I am beyond excited about this study because it provides a viable solution to young girls and women in whom vaginal structure and function has been compromised. Stem cell technologies for use in tissue biofabrication is where the future of reconstructive surgery lies,” Dr. Moalli said.
The Magee Summit is sponsored by UPMC and UPMC Health Plan, and the Magee Prize is sponsored by the Richard King Mellon Foundation. For additional information about the Magee Summit, the Magee Prize criteria and to register, please visit www.mageesummit.org.
Researchers Develop Coating for Endotracheal Tubes that Releases Antimicrobial Peptides
In a proof-of-concept study, researchers led by McGowan Institute for Regenerative Medicine affiliated faculty member Riccardo Gottardi, PhD, Assistant Professor of Pediatrics and head of the Bioengineering and Biomaterials Laboratory at the Children’s Hospital of Philadelphia (CHOP), have created a coating that can be applied to endotracheal tubes and release antimicrobial peptides that target infectious bacteria with specificity. The innovation could reduce upper-airway bacterial inflammation during intubation, a situation that can lead to chronic inflammation and a condition called subglottic stenosis, the narrowing of the airway by an accumulation of scar tissue. The findings were published in the journal The Laryngoscope.
“We have created a novel device to modulate the upper-airway microbiome, which could be used to prevent bacterial infections during intubation and help prevent subglottic stenosis and other airway diseases,” said senior study author Dr. Gottardi. “Not only does this technology work predictably and continuously over the normal duration of chronically intubated patients, but it is also fast and easy to produce and could easily be modulated to target any bacteria of interest.”
Recent studies have shown that the endotracheal microbiome of intubated patients with subglottic stenosis is unbalanced. However, addressing the overgrowth of certain bacteria with conventional antibiotics is not ideal, as their use can disrupt the balance of both “good” and “bad” bacteria, while also causing antimicrobial resistance.
Instead, the investigators explored the use of antimicrobial peptides (AMPs), which are small proteins that destabilize bacterial membranes, causing bacterial cells to fall apart and die. This mechanism of action allows them to target specific bacteria and makes them unlikely to promote antimicrobial resistance. Prior studies have shown that it is possible to coat endotracheal tubes with conventional antibiotics, so the research team investigated the possibility of incorporating AMPs into polymer-coated tubes to inhibit bacterial growth and modulate the upper-airway microbiome.
The researchers, led by Matthew Aronson, a graduate student in Penn Engineering’s Department of Bioengineering, tested their theory by creating a polymer coating that would release Lasioglossin-III, an AMP with broad-spectrum antibacterial activity. They found that Lasio released from coated endotracheal tubes, reached the expected effective concentration rapidly and continued to release at the same concentration for a week, which is the typical timeframe that an endotracheal is used before being changed. The investigators also tested their drug-eluting tube against airway microbes, including S. epidermidis, S. pneumoniae, and human microbiome samples and observed significant antibacterial activity, as well as prevention of bacterial adherence to the tube.
“This study shows that it is possible to create a drug-eluting endotracheal tube to prevent airway complications, which opens the door to future research on targeting specific pathogens that are responsible for laryngotracheal stenosis,” said study co-author Ian N. Jacobs, MD, Medical Director of the Center for Pediatric Airway Disorders in the Division of Otolaryngology and Endowed Chair in Pediatric Otolaryngology and Pediatric Airway Disorders at CHOP. “Moreover, the ability to purposefully select AMPs against certain microbes in the trachea and other organs could have significant implications in the prevention of specific diseases, even beyond airway disorders.”
The study was supported in part by the Ri.MED Foundation, the Children’s Hospital of Philadelphia Research Institute, the Frontier Program in Airway Disorders of the Children’s Hospital of Philadelphia, and the National Science Foundation Graduate Research Fellowship No. DGE 1845298.
Kozai Lab Student Receives NIH F99/K00 Pre-To-Postdoc Award to Improve Brain Implants
Steven Wellman, a bioengineering PhD candidate at the University of Pittsburgh, received a Predoctoral to Postdoctoral Fellow Transition Award (F99/K00) from the National Institutes of Health for his work with neural interfacing technology. These revolutionary devices have the potential to significantly advance our understanding of brain function and enable researchers to restore motor and sensory control lost from neurological disorders.
Mr. Wellman is a member of the BIONIC Lab at Pitt’s Swanson School of Engineering, which is led by McGowan Institute for Regenerative Medicine affiliated faculty member Takashi Kozai, PhD, assistant professor of bioengineering. His doctoral work focuses on the limitations of penetrating brain microelectrodes and the mechanisms that contribute to device failure.
“Despite the incredible potential of this technology to improve human health, the efficacy of intracortical microelectrodes for clinical therapy is limited by an inability to detect or modulate neurons over time and is presumed to be due to severe bodily reactions to a foreign object,” he said.
Researchers have yet to determine the biological mechanisms behind device failure, but recent studies suggest that neurovascular dysfunction may play a role in progressive neuron loss and tissue failure after implantation. Mr. Wellman studies how pericytes, specialized cells that work closely with cerebral blood vessels in the brain, contribute to this process.
“Neurovascular health and function are governed in part by perivascular pericytes,” he explained. “These cells demonstrate important roles in regulating vascular tone, blood-brain barrier integrity, and neuroimmune functions and have become increasingly recognized as prominent figures in the pathogenesis of brain inflammation and disease.”
In his project, Mr. Wellman examines how the structure and function of brain pericytes are altered during microelectrode implantation and subsequently affect neuronal health and neurovascular function. To do so, he uses a combination of two-photon imaging, electrophysiology, adeno-associated viruses (AAVs), and optogenetics within mice.
He also studies how pericyte activity can be modulated to improve neurovascular function and tissue health following brain injury. The results of this work could impact future therapies aimed at improving electrode-tissue integration, device performance and fidelity, and neurodegenerative brain injuries and diseases.
“The human health benefits of neural interfacing technology are highlighted by their translational potential from bench-to-bedside,” Mr. Wellman added. “At the benchside, microelectrodes are an effective tool enabling neuroscientists to interface bi-directionally with neuronal, glial, and vascular cells within the brain in order to understand their physiological and pathological roles.
“At the bedside, researchers have demonstrated the clinical power of neural microelectrodes as part of brain-computer interfaces (BCIs) for human rehabilitation by restoring motor control to tetraplegic patients and, more recently, going as far as re-establishing sensory input (haptic feedback) through bi-directional neuroprostheses.”
Mr. Wellman’s work will not only impact the field of brain-computer interfaces, but it will also branch into other areas of brain research in which pericyte and vascular dysfunction are present, including ischemia, hemorrhagic stroke, cerebrovascular disease, and Alzheimer’s disease (AD).
“Ultimately, my long-term career goal is to apply these advanced neurotechnologies and experimental methodologies to better understand and treat progressive neurodegenerative disease, particularly AD, in which neurovascular injury and dysfunction can figure prominently,” Mr. Wellman said.
Illustration: University of Pittsburgh Swanson School of Engineering (Wellman)/McGowan Institute for Regenerative Medicine (Kozai)
Exploring Silk’s Full Potential

From ski slopes to Girl Scouts, McGowan Institute for Regenerative Medicine affiliated faculty member Rosalyn Abbott’s classroom of choice has evolved over the years, but her love for teaching and discovery remains a steady constant. On any given day, she can be found integrating biomaterials, namely silk, with tissue engineering techniques in her lab, or teaching introductory engineering courses to undergraduate students at Carnegie Mellon University (CMU). Her group’s latest research uncovered a novel finding—that silk scaffolding is responsive to ultrasound.
Silk is a safe, unique, and versatile natural biomaterial that has successfully been used in wound healing and in tissue engineering of cartilage, tendon, and ligament tissues. It can easily be extracted from several sources, most commonly a Bombyx mori cocoon, and from there, processed into different formats including gels, scaffolds, and films.
“We call silk a ‘blank slate’ because it has the potential to be used in so many different applications,” explained Dr. Abbott, an assistant professor of biomedical engineering with a courtesy appointment in materials science and engineering at CMU. “Not only can you alter silk’s mechanical properties, but also, you can adjust its degradation rate, or in other words, how quickly or slowly silk scaffolding material breaks down in the body as it is replaced by new tissue.”
Dr. Abbott’s lab uses silk to engineer adipose (fat) tissue depots for filling soft tissue defects and for modelling diseases. This work fits into the bigger picture field of tissue engineering, or the practice of combining scaffolds, cells, and biologically active molecules into functional tissues. Ultimately, the aim is to assemble functional constructs that restore, maintain, or improve damaged tissues or whole organs.
Currently, there is no method of determining a patient’s regenerative rate prior to implanting a biomaterial, nor is there a way to adjust the degradation once the material has been implanted. Patients regenerate tissues at different rates, depending on such factors as age, nutritional status, disease state, lifestyle, gender, etc. A mismatch in regenerative rate and biomaterial degradation leads to inappropriate immune responses and poor healing of the implant.
In recent work published in Advanced Healthcare Materials, Dr. Abbott’s group investigated the use of non-invasive, therapeutic ultrasound to trigger and adjust silk scaffold degradation post-implantation. They showed that ultrasound exposure could successfully decrease weight, while increasing porosity of silk scaffolds—without affecting the health or metabolism of cells within the tissues. They also tracked scaffold degradation with imaging ultrasound as a proof-of-concept that a clinician could monitor the degradation and adjust the scaffold properties, as needed, on-demand. McGowan Institute affiliated faculty member Keith Cook, PhD, interim department head and professor of biomedical engineering at CMU, is a co-author on this study.
These findings are clinically relevant for tissue engineering approaches that implant silk biomaterials to restore structure, while tissues slowly grow into the space and replace the scaffold material.
Next, Dr. Abbott’s group plans to research and test a broader range of degradation profiles to ultimately create more responsive biomaterials. Megan DeBari, lead author of the recent Advanced Healthcare Materials paper and an MSE PhD student in Dr. Abbott’s lab, is pursuing a startup company to further develop the approach, through an Innovation Fellowship with Carnegie Mellon’s Swartz Center for Entrepreneurship.
Long-term, Dr. Abbott is working toward the development of a personalized biomaterial platform, where biomaterial degradation can be adjusted with focused ultrasound following routine monitoring of how a patient is healing.
“One of the aspects of teaching and research that excites me is the continued resilience and tenacity of the students I have the privilege of working with,” shared Dr. Abbott. “It’s not for the faint of heart, but I’ve had such rewarding interactions with my students, and diversity is an important aspect of that. Whether it’s me or another expert presenting in one of my classes, it’s important to me that my students see a version of themselves represented by leadership in the classroom.”
Watch Dr. Abbott explain her research here.
Dr. Elizabeth Wayne Awarded NIH R35 Grant for Macrophage Polarization Research

McGowan Institute for Regenerative Medicine affiliated faculty member and Carnegie Mellon University Chemical and Biomedical Engineering Assistant Professor, Elizabeth Wayne, PhD, has been awarded an NIH R35 grant, otherwise known as the Maximizing Investigators’ Research Award (MIRA), providing her with $1.7 million in funding over five years.
According to NIH, MIRA is awarded to the nation’s most talented and promising investigators. It aims to provide researchers with more flexibility and stability, enhancing scientific productivity and increasing the chance for significant breakthroughs.
“This grant is a huge honor and achievement for me,” said Dr. Wayne.
“As a junior faculty member, it will allow me to pursue groundbreaking research ideas quickly and help me build the kind of research program that I have been dreaming of for so long.”
The grant provides Dr. Wayne and her group the resources needed to develop bioluminescence microscopy technology to measure macrophage polarization responses in real-time. Her platform will evaluate the intrinsic and extracellular environmental stimuli that are most important for sensing macrophage polarization in a diseased environment context.
Macrophages are a type of white blood cell in the immune system that support routine tissue maintenance, like destroying foreign pathogens (such as viruses or bacteria) and digesting dead cells. Like shifting gears on a bike, macrophages cycle between these functions by adjusting their behavior based on the present environmental signals. How well a macrophage can shift gears, or polarize, is universally implicated in disease, from cancer to Alzheimer’s disease to healing following a spinal cord injury. However, the ability to measure macrophage polarization in real-time is challenging, making it difficult to monitor the success of therapies like biomaterial implants or nanoparticle drug delivery systems.
“My research is fundamentally about understanding how immune cells, like macrophages, decide how to respond to something like a virus or cancer cell,” said Dr. Wayne.
“If successful, this information can be used by doctors to design new therapies or even make biomaterials that can direct tissue regeneration,” added Dr. Wayne.
In Dr. Wayne’s lab, preliminary data shows that bioluminescence microscopy can deliver data, that when combined with the cell tracking capabilities of traditional imaging, will allow scientists to measure macrophage polarization accurately.
“This research will help us understand how to develop therapies, personalized to the patient’s unique macrophage functional signature, and could lead to the development of better real-time biological sensors, which would ultimately improve patient outcomes.”
To accomplish these goals, Dr. Wayne’s lab will employ ex-vivo culture systems and live bioluminescence imaging to identify novel strategies for measuring macrophage polarization and validate the importance of analyzing polarization in a disease context.
Dr. Wayne hopes this research will lead to new strategies for synthetic biology development, enhancement of diagnostic testing and help develop new therapeutic targets. In addition, the knowledge and tools acquired will be applied to other cells where polarization is paramount, such as stem cell differentiation, chemoattraction, and cell metabolism.
AWARDS AND RECOGNITION
Dr. Steven Little Named Distinguished Professor

McGowan Institute for Regenerative Medicine faculty member Steven Little, PhD, internationally recognized for his research in pharmaceutics and biomimetic drug delivery systems, now adds the University of Pittsburgh’s highest distinction for faculty to his list of honors. Recognizing his contributions to the professoriate as well as research, scholarly impact, and leadership, Dr. Little was appointed Distinguished Professor by Chancellor Patrick Gallagher.
Dr. Little, who also serves as the William Kepler Whiteford Endowed Professor and Department Chair of Chemical and Petroleum Engineering in Pitt’s Swanson School of Engineering, has developed numerous new drug formulations including controlled drug release that mimics the body’s own mechanisms of healing and resolving inflammation. Unlike traditional medications that require large doses administered via ingestion, inoculation or intravenously, biomimetic treatments recruit a patient’s own cells to treat disease at the source. In particular, Dr. Little’s research shows potential new applications for glaucoma, gum disease, and even transplant organ rejection.
“Steve is a truly outstanding individual whose academic and research career trajectory has made a remarkable impact in his field, but also among his fellow academicians and the many students he has taught and mentored,” noted James Martin II, PhD, U.S. Steel Dean of Engineering at Pitt. “To attain such recognition from the University when he is only at the midpoint of his career is a recognition of his dedication, creativity, and passion for engineering education and research.”
Since joining the Pitt faculty in 2006 after his doctoral training, Dr. Little has secured nearly $30 million in peer-reviewed funding from federal sources such as the National Science Foundation (NSF), National Institutes of Health (NIH), Department of Energy, and Department of Defense. His publication record includes more than 100 high-impact publications in Journal of the American Chemical Society, Angewandte Chemie, Science Advances, Proceedings of the National Academy of Sciences, ACS Nano, Advanced Materials, Biomaterials, and two separate feature review articles in Journal of Materials Chemistry. His work has been highlighted several times by Nature, Nature Methods, NIH, NSF, and several local and national media sources including the Wall Street Journal.
McGowan Institute faculty member Harvey Borovetz, PhD, Distinguished Professor and Former Chair of Bioengineering at Pitt, who chaired Dr. Little’s nomination committee noted, “It is a tremendous accomplishment for an academic to be recognized as Distinguished Professor at the zenith of their career, and even more rare for someone to be so honored in such short time. Dr. Little’s impact is far-reaching, not only within his field but regarding the growth of his own department at Pitt.”
Through his seven-year tenure as Chair, the Department of Chemical and Petroleum Engineering has seen over a two-fold increase in grant proposal submissions, approximately a two-fold increase in peer-reviewed publications, an increase of undergraduate revenue generation of nearly 60 percent, and an increase in net graduate tuition generation of 175 percent. Supporting this growth, he has hired 14 new faculty members and five staff, increasing the Department’s faculty size by over 60 percent.
“Steve’s research cuts across the traditional boundaries of scientific disciplines, an area where he clearly thrives,” noted Robert Langer Jr., PhD, one of Dr. Little’s references and his PhD advisor at the Massachusetts Institute of Technology (MIT). “In this way, he is a superb example of a modern-day young innovator who attacks problems from different perspectives when compared to his peers.” Dr. Langer currently is the David H. Koch Institute Professor at MIT.
“I am honored and humbled to have been nominated for this caliber of appointment and to have been supported by so many at the Distinguished Rank from around the world,” Dr. Little said. “It’s been those people who have inspired me to innovate and train the next generation of scientists. I can only hope to support others the way that they have supported me.”
Congratulations, Dr. Little!
Illustration: University of Pittsburgh Swanson School of Engineering.
Dr. Xi (Charlie) Ren Receives National Academy of Medicine Award

The National Academy of Medicine (NAM), together with eight global collaborators representing over 50 countries and territories, recently announced the awardees of the 2021 Healthy Longevity Catalyst Awards. These awards are part of the Healthy Longevity Global Competition, a multiyear, multistage, and multimillion-dollar international competition seeking potential breakthrough innovations aiming to extend human health and function later in life.
McGowan Institute for Regenerative Medicine affiliate faculty member Xi (Charlie) Ren, PhD, assistant professor in the Department of Biomedical Engineering at Carnegie Mellon University, was named a U.S. Catalyst Award Winner for his project entitled “Enabling Healthy Longevity by Investigating the Aging Extracellular Environment.” He will receive $50,000 as seed funding to help advance his idea.
NAM administers the U.S.-based Catalyst Award competition, for which approximately 500 innovators submitted applications in 2021. Twenty-five submissions received Catalyst Awards from the NAM this year.
The National Academy of Medicine, established in 1970 as the Institute of Medicine, is an independent organization of eminent professionals from diverse fields including health and medicine; the natural, social, and behavioral sciences; and beyond. It serves alongside the National Academy of Sciences and the National Academy of Engineering as an adviser to the nation and the international community. Through its domestic and global initiatives, the NAM works to address critical issues in health, medicine, and related policy and inspire positive action across sectors. The NAM collaborates closely with its peer academies and other divisions within the National Academies of Sciences, Engineering, and Medicine.
Congratulations, Dr. Ren!
Dr. Rory Cooper Receives Pennsylvania Veterans Service Award

Recently, leaders of the Pennsylvania National Guard awarded McGowan Institute for Regenerative Medicine affiliated faculty member Rory Cooper, PhD, FISA & Paralyzed Veterans of America Professor and Distinguished Professor of the Department of Rehabilitation Science & Technology, Professor of Bioengineering, Physical Medicine & Rehabilitation, and Orthopedic Surgery at the University of Pittsburgh, and Founding Director and VA Senior Research Career Scientist of the Human Engineering Research Laboratories (HERL), and Garrett Grindle, PhD, Associate Director for Engineering at HERL and a Research Scientist at the University of Pittsburgh, the Pennsylvania Veterans Service Award for their work protecting veterans and their caregivers during the pandemic.
In April 2020, HERL pivoted from their usual technology research and development to producing nasal swabs, face shields, and other medical supplies to meet demand during the crisis. Their work helped keep VA hospitals open and safe for workers, patients, and caregivers.
“I am extremely proud of the team at HERL,” Dr. Cooper told the VA’s Research Currents publication last spring. “They have risen to the challenge of assisting with VA’s response to COVID-19 and have performed outstandingly. The work of the team at HERL has likely helped slow the spread of the disease and has assisted VA health care providers in saving the lives of veterans.”
Congratulations!
Illustration: HERL.
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#226 –– Dr. Heth Turnquist discusses his research in cytokine and regulatory cell networks in transplantation.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
PUBLICATION OF THE MONTH
Author: Bilge E Öztürk, Molly E Johnson, Michael Kleyman, Serhan Turunç, Jing He, Sara Jabalameli, Zhouhuan Xi, Meike Visel, Valérie L Dufour, Simone Iwabe, Felipe Pompeo Marinho, Gustavo D Aguirre, José-Alain Sahel, David V Schaffer, Andreas R Pfenning, John G Flannery, William A Beltran, William R Stauffer, Leah C Byrne
Title: scAAVengr, a transcriptome-based pipeline for quantitative ranking of engineered AAVs with single-cell resolution
Summary: Background: Adeno-associated virus (AAV)-mediated gene therapies are rapidly advancing to the clinic, and AAV engineering has resulted in vectors with increased ability to deliver therapeutic genes. Although the choice of vector is critical, quantitative comparison of AAVs, especially in large animals, remains challenging.
Methods: Here, we developed an efficient single-cell AAV engineering pipeline (scAAVengr) to simultaneously quantify and rank efficiency of competing AAV vectors across all cell types in the same animal.
Results: To demonstrate proof-of-concept for the scAAVengr workflow, we quantified – with cell-type resolution – the abilities of naturally occurring and newly engineered AAVs to mediate gene expression in primate retina following intravitreal injection. A top performing variant identified using this pipeline, K912, was used to deliver SaCas9 and edit the rhodopsin gene in macaque retina, resulting in editing efficiency similar to infection rates detected by the scAAVengr workflow. scAAVengr was then used to identify top-performing AAV variants in mouse brain, heart and liver following systemic injection.
Conclusions: These results validate scAAVengr as a powerful method for development of AAV vectors.
Source: eLife 2021;10:e64175 DOI: 10.7554/eLife.64175
GRANT OF THE MONTH
PI: Andrew Duncan
Title: Mechanisms of Liver Regeneration Induced by Acetaminophen Toxicity
Description: Liver disorders affect 30 million people in the United States and are the country’s 10th leading cause of death. To improve liver disease treatments, a better understanding of hepatocyte biology is required. The liver contains diploid and polyploid hepatocytes, with polyploids comprising nearly 50% adult human and 90% adult mouse hepatocytes. The functional differences between diploid and polyploid hepatocytes are poorly understood. We previously demonstrated that diploid hepatocytes facilitate rapid liver regeneration, but it remains unknown how diploid and polyploid hepatocytes respond to drug-induced injury. Acetaminophen (APAP) is a common analgesic that can cause acute liver injury, resulting in liver failure and death when taken in excess. When APAP overdose causes extensive centrilobular hepatocyte death, the liver undergoes compensatory proliferation and recovers if the ratio of necrosis to regeneration is low. To investigate the role diploid and polyploid hepatocytes in vivo, we utilize E2f7 and E2f8 liver-specific knockout mice (LKO) where E2f7 and E2f8 are deleted during postnatal development; these mice are functionally normal through 6-9 months of age but are depleted of polyploid hepatocytes (LKO livers are >70% diploid). Preliminary studies indicate that LKO mice enriched with diploid hepatocytes are less damaged and recover faster from APAP injury than wild-type (WT) mice enriched with polyploid hepatocytes. The Grantee shall investigate mechanisms of liver injury and regeneration during APAP-induced liver injury and failure. This project shall determine ploidy-dependent and ploidy-independent mechanisms of liver repair and regeneration following APAP overdose.
Source: Commonwealth of Pennsylvania
Term: 7/1/2021-6/30/22
Amount: $77,260
