May 2017 | VOL. 16, NO. 5| www.McGowan.pitt.edu
Precision Medicine Improves Treatment Outcomes for Some Pancreatic Cancer Patients

University of Pittsburgh and UPMC researchers are paving the way for genome-targeted treatments in pancreatic cancer, an especially deadly form of cancer with few existing therapeutic options, according to a pair of recent studies.
The first study used genomic profiling to identify targeted therapies that resulted in benefits for patients with pancreatic cancer, including one whose tumor contained a mutation in the anaplastic lymphoma kinase (ALK) gene. In the second study, researchers used existing drugs already treating other types of ALK-mutated cancers to improve outcomes in pancreatic cancer patients with the same genetic alterations.
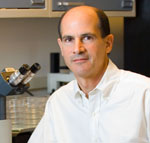
“Together, these two findings begin to capture the promise of precision medicine in pancreatic cancer, which has so far not experienced the same success with targeted treatments as other cancer types,” said the senior author of both studies, Nathan Bahary, MD, PhD, associate professor of medicine at Pitt, co-director of the UPMC Pancreatic Cancer Center of Excellence, and McGowan Institute for Regenerative Medicine affiliated faculty member. “The assessment of these actionable alterations is now part of routine pancreatic cancer care at UPMC.”
As the third-leading cause of cancer deaths in the United States, and with a 5-year survival rate of just 8 percent, pancreatic cancer is one of the most lethal forms of the disease. Currently available treatments are largely ineffective, so there is a desperate need for better therapeutic options, explained Dr. Bahary.
In the first study, published in the January issue of Cancer Medicine, first author Mashaal Dhir, MD, an oncologic surgical fellow at UPMC, and colleagues used DNA sequencing to look for gene changes in over 100 patient samples of advanced gastrointestinal cancers, including colorectal and pancreatic tumors.
They identified several mutations in each cancer type and used that information to make treatment recommendations in 38 percent of cases. Approximately 14 percent of patients could receive the recommended therapy due to rapid decline in the other patients. However, half of those who received genomic-guided therapy experienced significant clinical benefit with improvement in overall survival, which would not have been possible on standard-of-care therapies. This suggests that mutational analyses done earlier during therapy may provide benefit to more patients, the authors said.
One patient’s pancreatic tumor had a mutation in the ALK gene. Genetic mutations involving ALK have been identified in several different types of cancer, including those of the breast, colon, and lung, and drugs targeting this pathway have been successfully used for treatment of these tumors.
The second study, published online in the Journal of the National Comprehensive Cancer Network (JNCCN), took a closer look at ALK mutations in pancreatic cancer. Co-lead authors Aatur Singhi, MD, PhD, assistant professor of pathology at UPMC, and Siraj Ali, MD, PhD, director of clinical development and medical affairs, Foundation Medicine Inc., Cambridge, Massachusetts, performed comprehensive genomic profiling of more than 3,000 pancreatic cancers.
Alterations in the ALK gene were present in five patients (0.2 percent). Four of these five were treated with drugs that inhibit ALK, and three experienced a positive response, as evidenced by either stable disease, tumor shrinkage, or a reduction in levels of a pancreatic cancer biomarker.
Patients with pancreatic cancer are typically diagnosed late in life, at an average age of 71. Patients with ALK mutations averaged just 38 years at diagnosis. The prospect of having an effective and clinically available treatment to offer a small subset of pancreatic cancer patients, a population with so few options, is extremely encouraging, said Dr. Bahary. The new work also highlights the importance of ALK mutation screening in young pancreatic cancer patients.
The new studies also have much broader implications for pancreatic cancer.
“Modern DNA sequencing techniques have brought with them the hope of targeting anti-cancer therapies to a particular cancer’s vulnerabilities,” Dr. Bahary said. “However, the potential of these precision medicine initiatives has not yet been achieved in pancreatic cancer. Beyond ALK mutations, our two studies describe some of the initial steps needed to utilize targeted therapies more generally in pancreatic cancer.”
RESOURCES AT THE MCGOWAN INSTITUTE
June Histology Special
Verhoeff-Van Gieson (VVG)
Elastin is a protein in connective tissue that allows many tissues in the body to resume their shape after stretching or contracting. Elastin helps skin to return to its original position when it is poked or pinched.
Elastin serves an important function in arteries as a medium for pressure wave propagation to help blood flow and is particularly abundant in large elastic blood vessels such as the aorta. Elastin is also very important in the lungs, elastic ligaments, the skin, and the bladder, elastic cartilage. It is present in all vertebrates above the jawless fish.
Verhoeff’s stain forms a variety of cationic, anionic and non-ionic bonds with elastin, the main constituent of elastic fiber tissue. Elastin has a strong affinity for the iron-hematoxylin complex formed by the reagents in the stain and will hence retain dye longer than other tissue elements, which allows elastin to remain stained while other tissue elements are decolorized. Elastic fibers and cell nuclei are stained black, collagen fibers are stained red, and other tissue elements including cytoplasm are stained yellow.
 You’ll receive 25% off your VVG stain every day in June. Contact Lori at the McGowan Core Histology Lab and ask about our VVG specials. Email perezl@upmc.edu or call 412-624-5265. As always, you will receive the highest quality histology in the quickest turn-around time.
You’ll receive 25% off your VVG stain every day in June. Contact Lori at the McGowan Core Histology Lab and ask about our VVG specials. Email perezl@upmc.edu or call 412-624-5265. As always, you will receive the highest quality histology in the quickest turn-around time.
Did you know the more samples you submit to the histology lab the less you pay per sample?
Contact Lori to find out how!
Using Flow Cytometry to Help Characterize the Functional Role of Polyploid Hepatocytes
In the laboratory of McGowan Institute for Regenerative Medicine faculty member Andrew Duncan, PhD, Assistant Professor in the Department of Pathology at the University of Pittsburgh, team members Patrick Wilkinson, 3rd Year CMP Graduate Student, and Frances Alencastro, Lab Manager, sought the expertise of Lynda Guzik, Manager of the McGowan Institute Flow Cytometry Core Facility, to design and perform some of their research experiments using flow cytometry. A description of their collaboration follows:
Hepatocytes are characterized by variations in chromosome content known as polyploidy. Polyploidy is defined as an increase in the entire chromosome set within the cell. For example, in humans, diploid (2n) cells contain 46 chromosomes while polyploid cells that are tetraploid (4n) contain 92 chromosomes. Interestingly, polyploid hepatocytes comprise >90% of hepatocytes in adult mice and 50% in adult humans. The goal of the lab is to characterize the functional role of polyploid hepatocytes in the context of liver function and regeneration.
To study the differences between diploid and polyploid hepatocytes the researchers utilized liver-specific knockout mice lacking transcription factors E2f7 and E2f8 (E2f7/E2f8-lko). The analyses revealed E2f7/E2f8-lko mice contain 10 times more diploid hepatocytes and 3- to 10-fold fewer polyploid cells compared to controls. Ms. Guzik collaborated with the team to design and perform an experiment that would enable them to determine if the ploidy defect was stable. For this assay, they transplanted E2f7/E2f8-lko hepatocytes from adult (2 months) donors into Fah-/- recipients, a liver repopulation model.
After isolating the hepatocytes from the repopulated livers, flow cytometry was used to discriminate between the donor and host hepatocytes, and determine the ploidy states of the repopulated livers. Since the host and donor cells had different murine MHC haplotypes the team could differentiate between them by staining the hepatocytes with antibodies against the H-2Kq antigen (donor cells) and H-2Kd antigen (host cells). The flow analyses revealed that >90% of the cells in the repopulated livers were H-2Kq+, indicating that hepatocytes from E2f7/E2f8-control and knockout mice successfully repopulated the livers of the host mice (Figures 1A and 2A). The team’s ploidy analyses revealed the livers repopulated with E2f7/E2f8-control cells contained predominantly polyploid (4c and 8c) hepatocytes (Figure 1B). This was expected as wild-type hepatocytes readily polyploidize during liver repopulation. However, most cells in the livers repopulated with E2f7/E2f8-lko donors were diploid (2c) hepatocytes (Figure 2B). This indicated that the E2f7/E2f8-lko hepatocytes did not polyploidize during liver repopulation. Therefore, the flow analyses revealed that the E2f7/E2f8-lko ploidy defect was stable and E2f7/E2f8-lko hepatocytes do not polyploidize when forced to undergo multiple rounds of cell division.
Mr. Wilkinson and Ms. Alencastro are thankful for the expertise and assistance provided by Ms. Guzik in developing, optimizing, and performing this experiment, and look forward to continued work with the McGowan Institute Flow Cytometry Core for future hepatic ploidy analyses.
If you have a research project where flow cytometry may benefit your efforts, please feel free to contact Lynda Guzik for more information.
McGowan Flow Facility Updates Policy
Thanks to our researchers, the McGowan Flow Facility has had a very productive year. Scheduled appointment time has doubled in the past 6months. As some researchers have recently realized, appointment requests for ‘next week’ can no longer be accommodated as easily as they once were. In order to better serve you and respect everyone’s valuable time and work, we feel it is necessary to adapt our current scheduling and billing policy to better utilize the available time on the Aria cell sorter. No changes are currently planned for the Quant. Changes will become effective on July 1, 2017 and can be accessed on our website.
For details about the new policy, please click here.
SCIENTIFIC ADVANCES
Protein Primes Mouse Stem Cells to Quickly Repair Injury, Study Finds
 Like drag car racers revving their engines at the starting line, stem cells respond more quickly to injury when they’ve been previously primed with one dose of a single protein, according to a study from the Stanford University School of Medicine.
Like drag car racers revving their engines at the starting line, stem cells respond more quickly to injury when they’ve been previously primed with one dose of a single protein, according to a study from the Stanford University School of Medicine.
Mice given the priming protein recover muscle function more quickly after damage, their skin heals more rapidly, and even the shaved area around the injury regrows hair more quickly, the study found.
Harnessing the power of this protein may one day help people recover more quickly from surgery or restore youthful vigor to aging stem cells.
“We’re trying to better understand wound healing in response to trauma and aging,” said Thomas Rando, MD, PhD, professor of neurology and neurological sciences at Stanford and also an affiliated faculty member of the McGowan Institute for Regenerative Medicine. “We’ve shown that muscle and bone marrow stem cells enter a stage of alertness in response to distant injury that allows them to spring into action more quickly. Now we’ve pinpointed the protein responsible for priming them to do what they do better and faster.”
Dr. Rando, who also directs Stanford’s Glenn Center for the Biology of Aging, is the senior author of the study, which will be published in Cell Reports. Former postdoctoral scholar Joseph Rodgers, PhD, is the lead author. Dr. Rodgers is now an assistant professor of stem cell biology and regenerative medicine at the University of Southern California.
Potential therapy
“Our research shows that by priming the body before an injury you can speed the process of tissue repair and recovery, similar to how a vaccine prepares the body to a fight infection,” Dr. Rodgers said. “We believe this could be a therapeutic approach to improve recovery in situations where injuries can be anticipated, such as surgery, combat, or sports.”
Normally, adult, tissue-specific stem cells are held in a kind of cellular deep freeze called quiescence to avoid unnecessary cell division in the absence of injury. In a 2014 paper published in Nature, Drs. Rodgers and Rando showed in laboratory mice that an injury to the muscle of one leg caused a change in the muscle stem cells of the other leg. These cells entered what the researchers called an “alert” phase of the cell cycle that is distinct from either fully resting or fully active stem cells.
The fact that muscle stem cells distant from the injury were alerted indicated that the damaged muscle must release a soluble factor that can travel throughout the body to wake up quiescent stem cells. Dr. Rodgers and his colleagues found that a protein called hepatocyte growth factor, which exists in a latent form in the spaces between muscle cells and tissue, can activate a critical signaling pathway in the cells by binding to their surfaces. This pathway stimulates the production of proteins important in alerting the stem cells. But it wasn’t known how HGF itself became activated.
In the new study, Dr. Rodgers and his colleagues identified the activating factor by injecting uninjured animals with blood serum isolated from animals with an induced muscle injury. (Mice were anesthetized prior to a local injection of muscle-damaging toxin; they were given pain relief and antibiotics during the recovery period.) After 2.5 days, the researchers found that muscle stem cells from the recipient animals were in an alert state and completed their first cell division much more quickly than occurred in animals that had received blood serum from uninjured mice.
“Clearly, blood from the injured animal contains a factor that alerts the stem cells,” said Dr. Rando. “We wanted to know, what is it in the blood that is doing this?”
Increased levels of a protein
The researchers found that the serum from the injured animals had the same levels of HGF as the control serum. However, it did have increased levels of a protein called HGFA that activates HGF by snipping it into two pieces. Treating the serum with an antibody that blocked the activity of HGFA eliminated the recovery benefit of pretreatment, the researchers found.
In a related experiment, exposing the animals to a single intravenous dose of HGFA alone two days prior to injury helped the mice recover more quickly. They scampered around on their wheels sooner and their skin healed more quickly than mice that received a control injection.
They also regrew their hair around the shaved surgical site more completely than did the control animals.
“Just like in the muscles, we saw the responses in the skin were dramatically improved when the stem cells were alerted,” Dr. Rando said.
In addition to pinpointing possible ways to prepare people for surgeries or other situations in which they might sustain wounds, the researchers are intrigued by the role HGF and HGFA might play in aging. It’s known that the pathway activated by these proteins is less active in older people and animals.
“Stem cell activity diminishes with advancing age, and older people heal more slowly and less effectively than younger people. Might it be possible to restore youthful healing by activating this pathway?” said Dr. Rando. “We’d love to find out.”
The work is an example of Stanford Medicine’s focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Illustration: McGowan Institute for Regenerative Medicine.
Motor Neurons Adjust to Control Tasks, New Brain Research Reveals
 New research from Carnegie Mellon University’s College of Engineering and the University of Pittsburgh reveals that motor cortical neurons optimally adjust how they encode movements in a task-specific manner. The findings enhance our understanding of how the brain controls movement and have the potential to improve the performance and reliability of brain-machine interfaces, or neural prosthetics, that assist paralyzed patients and amputees. McGowan Institute of Regenerative Medicine affiliated faculty member Andrew Schwartz, PhD, distinguished professor of neurobiology and chair in systems neuroscience at the University of Pittsburgh School of Medicine and a member of the University of Pittsburgh Brain Institute, is a co-author on the study.
New research from Carnegie Mellon University’s College of Engineering and the University of Pittsburgh reveals that motor cortical neurons optimally adjust how they encode movements in a task-specific manner. The findings enhance our understanding of how the brain controls movement and have the potential to improve the performance and reliability of brain-machine interfaces, or neural prosthetics, that assist paralyzed patients and amputees. McGowan Institute of Regenerative Medicine affiliated faculty member Andrew Schwartz, PhD, distinguished professor of neurobiology and chair in systems neuroscience at the University of Pittsburgh School of Medicine and a member of the University of Pittsburgh Brain Institute, is a co-author on the study.
“Our brain has an amazing ability to optimize its own information processing by changing how individual neurons represent the world. If we can understand this process as it applies to movements, we can design more precise neural prostheses,” says Steven Chase, PhD, assistant professor in the Department of Biomedical Engineering and the Center for Neural Basis of Cognition. “We can one day, for example, design robotic arms that more accurately implement a patient’s intended movement because we now better understand how our brain adjusts on a moment-by-moment basis when we are in motion.”
The study explored the change in brain activity during simple motor tasks performed through virtual reality in both 2-D and 3-D. The researchers wanted to know if the motor cortical neurons would automatically adjust their sensitivity to direction when presented with a wide range of possible directions instead of a narrow one. Previous research in the field has suggested that this phenomenon, called dynamic range adaptation, is known to occur in neurons sensitive to sound, touch, and light — prompting the researchers to ask if the same phenomena would apply to neurons in the motor system that are associated with movement.
“When you walk out into the bright summer sun, you squint, and the neurons in your retina use dynamic range adaptation to automatically increase their sensitivity so that you can clearly see until the clouds pass over again,” explains Robert Rasmussen, MD/PhD student at the University of Pittsburgh School of Medicine and first author of the study. “This feature allows the brain to better encode information by using its limited resources efficiently. We wanted to find out if our brain encodes movement in the same way.”
The results revealed that dynamic range adaptation did indeed occur in the motor cortical neurons. Based on these findings, the researchers concluded that this feature is widespread throughout the brain.
“We found that dynamic range adaptation isn’t restricted to sensory areas of the brain. Instead, it is a ubiquitous encoding feature of the cortex,” explains Dr. Schwartz. “Our findings show that it is a feature of information processing, which your brain uses to efficiently process whatever information it is given — whether that is light, sound, touch, or movement. This is an exciting result that will motivate further research into motor learning and future clinical applications.”
Illustration: Carnegie Mellon University Materials Science and Engineering.
Dr. Anna Balazs to Lead DOD MURI Program Project
 The U.S. Department of Defense recently announced the awarding of their 2017 large, multi-university grants in their MURI program. One of the 23 awards will go to a team of researchers led by McGowan Institute for Regenerative Medicine affiliated faculty member Anna Balazs, PhD, Distinguished Professor of Chemical Engineering and the Robert v. d. Luft Professor, Department of Chemical & Petroleum Engineering, University of Pittsburgh. Dr. Balazs will serve as the PI on the project entitled “Adaptive Self‐Assembled Systems: Exploiting Multifunctionality for Bottom‐up Large Scale Engineering” with the team spanning the University of Pittsburgh, Harvard, Northwestern, and the University of Illinois. The award is for 5 years at $1.5 million per year.
The U.S. Department of Defense recently announced the awarding of their 2017 large, multi-university grants in their MURI program. One of the 23 awards will go to a team of researchers led by McGowan Institute for Regenerative Medicine affiliated faculty member Anna Balazs, PhD, Distinguished Professor of Chemical Engineering and the Robert v. d. Luft Professor, Department of Chemical & Petroleum Engineering, University of Pittsburgh. Dr. Balazs will serve as the PI on the project entitled “Adaptive Self‐Assembled Systems: Exploiting Multifunctionality for Bottom‐up Large Scale Engineering” with the team spanning the University of Pittsburgh, Harvard, Northwestern, and the University of Illinois. The award is for 5 years at $1.5 million per year.
“The Multidisciplinary University Research Initiative program, or MURI, supports research by funding teams of investigators that include more than one traditional science and engineering discipline in order to accelerate the research progress,” said Dale Ormond, principal director for research in the Office of the Assistant Secretary of Defense for Research and Engineering. “Most of the program’s efforts involve researchers from multiple academic institutions and academic departments.” Ormond also stated that, “MURI awards also support the education and training of graduate students in new, cutting-edge research.”
The highly competitive MURI program complements other DOD basic research efforts that support traditional, single-investigator university research grants. By supporting multidisciplinary teams with larger and longer awards in carefully chosen and timely research topics identified for their long-term importance, DOD and the military services enhance the potential for significant and sustained advancement of the research in critical areas.
The Army Research Office, the Air Force Office of Scientific Research, and the Office of Naval Research solicited proposals in 23 topic areas important to the DOD and the military services. In response to the initial solicitation the department received 315 white papers. After two rounds of merit-based reviews, a panel of DOD experts narrowed the proposals to 89 from which the 23 final awards were selected. Based on the proposals selected in the 2017 competition, 55 U.S. academic institutions are expected to participate in 2017 MURI program.
Over the past 30 years, DOD’s MURI program resulted in significant capabilities for our military forces and opened up entirely new lines of research. Notable examples include foundations in artificial intelligence, compressive sensing and automated scene recognition, ultracold atoms and advanced sensing and navigation, advances in optoelectronics and mid-infrared imaging technology, and direct brain-computer communication. These and other important technological advances from the MURI program have impact on current and future military capabilities as well as multiple applications in the commercial sector.
McGowan Institute Supports Elementary Science and Technology
 Stephen Badylak, DVM, PhD, MD, recently represented the McGowan Institute at an educational outreach activity held at McKnight Elementary School in the North Allegheny School District. Michelle Scarritt, PhD, and Abby Stahl explained to students and their families how different human anatomy systems function.
Stephen Badylak, DVM, PhD, MD, recently represented the McGowan Institute at an educational outreach activity held at McKnight Elementary School in the North Allegheny School District. Michelle Scarritt, PhD, and Abby Stahl explained to students and their families how different human anatomy systems function.
Dr. Scarritt explained how the lungs work after showing the kids the rodent lung bioreactor. Our intercostal muscles and diaphragm work in unison to lower the pressure in our chest cavity. The pressure of the air in our lungs is then higher causing them to expand.
Ms. Stahl and Dr. Scarritt demonstrated how humans breathe using rodent lungs in a bioreactor. The kids removed air from the bioreactor chamber (using a syringe) to create a vacuum that allowed the rodent lungs to inflate with air. When air was pushed back into the chamber, the lungs collapse.
They also talked about the function of our liver and how our cardiovascular system works.
 Dr. Scarritt received her PhD from Tulane University in New Orleans, LA, where she studied lung tissue engineering. Through her experience with lung decellularization and recellularization within bioreactors, Dr. Scarritt now hopes to develop vascularization strategies for liver engineering applications. She is also interested in assessing the rate of ECM turnover during recellularization as a means of predicting clinical outcomes for porcine organ scaffolds.
Dr. Scarritt received her PhD from Tulane University in New Orleans, LA, where she studied lung tissue engineering. Through her experience with lung decellularization and recellularization within bioreactors, Dr. Scarritt now hopes to develop vascularization strategies for liver engineering applications. She is also interested in assessing the rate of ECM turnover during recellularization as a means of predicting clinical outcomes for porcine organ scaffolds.
Abby Stahl is an undergraduate at the University of Pittsburgh studying bioengineering with a concentration in cellular and tissue engineering. Her current research interests are focused on engineering functional liver tissue by developing novel methods of seeding hepatic cells within a 3-dimensional scaffold composed of extracellular matrix.
McGowan Institute Spin-Out Company Closes $36 Million Financing
 Based on core technology developed by McGowan Institute of Regenerative Medicine faculty members William Federspiel, PhD, W.K. Whiteford professor of bioengineering, chemical engineering, and critical care medicine, and the late Brack Hattler, MD, ALung Technologies, Inc., is today a leading provider of low-flow extracorporeal carbon dioxide removal (ECCO2R) technologies for treating patients with acute respiratory failure. The company announced recently the closing of a $36 million Series C financing, including existing convertible notes. The round was led by Philips and UPMC, through its innovation and commercialization arm UPMC Enterprises, with other new and existing investors participating. The funding will support a planned US-based pivotal trial for FDA approval of the company’s Hemolung Respiratory Assist System (RAS), a minimally invasive artificial lung device which removes carbon dioxide independently of the lungs through a process called Respiratory Dialysis®.
Based on core technology developed by McGowan Institute of Regenerative Medicine faculty members William Federspiel, PhD, W.K. Whiteford professor of bioengineering, chemical engineering, and critical care medicine, and the late Brack Hattler, MD, ALung Technologies, Inc., is today a leading provider of low-flow extracorporeal carbon dioxide removal (ECCO2R) technologies for treating patients with acute respiratory failure. The company announced recently the closing of a $36 million Series C financing, including existing convertible notes. The round was led by Philips and UPMC, through its innovation and commercialization arm UPMC Enterprises, with other new and existing investors participating. The funding will support a planned US-based pivotal trial for FDA approval of the company’s Hemolung Respiratory Assist System (RAS), a minimally invasive artificial lung device which removes carbon dioxide independently of the lungs through a process called Respiratory Dialysis®.
In 2015, the Hemolung RAS was granted Expedited Access Pathway (EAP) designation by the FDA, allowing ALung to collaborate more closely with the agency towards bringing the Hemolung technology to the United States. “Since 2013, hundreds of patients with acute respiratory failure have been successfully treated with the Hemolung RAS outside of the United States,” said Peter DeComo, ALung Chairman and CEO. “With this new financing, we will be able to conduct our US-based clinical trial, an important step towards obtaining FDA approval and making our device available to patients in the United States. We are grateful to Philips, UPMC, and our many other investors for their commitment to ALung and the numerous patients who stand to benefit from our technology.”
The investment by Philips and UPMC will bring more than capital to the company, with both organizations offering resources and expertise to support ALung’s work. ALung’s Board of Directors will be strengthened with new members from Philips and UPMC Enterprises. Adam Seiver, MD, will join the board as a representative from Philips, where he serves as the Chief Medical Officer of Philips Patient Care and Monitoring Systems. Joining from UPMC will be Jeanne Cunicelli, Executive Vice President of UPMC Enterprises. Ms. Cunicelli has more than two decades of investment and advising experience in the life sciences industry.
“We are excited to partner with ALung, whose mission reflects our own: to dramatically improve patient outcomes and the cost-effectiveness of care by applying cutting-edge science and technology,” said Steven Shapiro, MD, Chief Medical and Scientific Officer of UPMC. UPMC was the first hospital system in the United States to use the Hemolung RAS on an emergency use basis.
“As a leader in non-invasive ventilation solutions for the hospital and the home, we are committed to making a difference in patient care through innovation,” said Dr. Adam Seiver, Chief Medical Officer of Philips Patient Care and Monitoring Systems. “We see the potential of ALung’s innovative technology, and we are excited to partner with them and bring the technology to the next level.”
Joining Philips and UPMC in the Series C round were new and existing investors including Abiomed, The Accelerator Fund, Allos Ventures, Birchmere Ventures, Blue Tree Ventures, and Riverfront Ventures. Raymond James & Associates, Inc., acted as lead placement agent for the transaction.
Illustration: ALung Technologies, Inc.
Medical 3D Printing Applications
 McGowan Institute for Regenerative Medicine Director William Wagner, PhD, Professor of Surgery, Bioengineering and Chemical Engineering at the University of Pittsburgh, Chairman of the Tissue Engineering and Regenerative Medicine International Society (TERMIS) – Americas, Deputy Director of the NSF Engineering Research Center on Revolutionizing Metallic Biomaterials, and Chief Scientific Officer of the Armed Forces Institute of Regenerative Medicine, was a member of the keynote panel of the recently held RAPID + TCT, North America’s preeminent event for discovery, innovation, and networking in 3D manufacturing.
McGowan Institute for Regenerative Medicine Director William Wagner, PhD, Professor of Surgery, Bioengineering and Chemical Engineering at the University of Pittsburgh, Chairman of the Tissue Engineering and Regenerative Medicine International Society (TERMIS) – Americas, Deputy Director of the NSF Engineering Research Center on Revolutionizing Metallic Biomaterials, and Chief Scientific Officer of the Armed Forces Institute of Regenerative Medicine, was a member of the keynote panel of the recently held RAPID + TCT, North America’s preeminent event for discovery, innovation, and networking in 3D manufacturing.
Dr. Wagner served on the Panel: Medical 3D Printing Applications—Growth Beyond Surgical Guides. With anatomical models and surgical guides closer to standards of care, and device manufacturers taking advantage of the unique structures additive manufacturing can build, new applications are growing in the biomaterials area. Dr. Wagner and the other panelists discussed some of these applications, the developments making them possible, the similarities and differences between 3D printing with biomaterials and bioprinting, and expectations for impacting patient care.
RAPID + TCT is an additive manufacturing event that showcases product innovations and offers collaborative learning opportunities to ultimately accelerate the adoption and advancement of the technology. The two industry leaders in 3D technology events, SME and Rapid News Publications Ltd., combined their nearly 30 years of insights and experience to produce the annual RAPID + TCT event starting in 2017 in Pittsburgh, Pennsylvania.
Novel Gene Editing Approach to Cancer Treatment Shows Promise in Pre-Clinical Tests
 A novel gene therapy using CRISPR genome editing technology effectively targets cancer-causing “fusion genes” and improves survival in mouse models of aggressive liver and prostate cancers, University of Pittsburgh School of Medicine researchers report in a study published online recently in Nature Biotechnology. McGowan Institute for Regenerative Medicine affiliated faculty members George Michalopoulos, MD, PhD, Professor and Chairman of the Department of Pathology at the University of Pittsburgh, and Satdarshan Monga, MD, Endowed Research Chair in Experimental Pathology and the Vice-Chair of the Division of Experimental Pathology, Department of Pathology at Pitt, are co-authors on the study.
A novel gene therapy using CRISPR genome editing technology effectively targets cancer-causing “fusion genes” and improves survival in mouse models of aggressive liver and prostate cancers, University of Pittsburgh School of Medicine researchers report in a study published online recently in Nature Biotechnology. McGowan Institute for Regenerative Medicine affiliated faculty members George Michalopoulos, MD, PhD, Professor and Chairman of the Department of Pathology at the University of Pittsburgh, and Satdarshan Monga, MD, Endowed Research Chair in Experimental Pathology and the Vice-Chair of the Division of Experimental Pathology, Department of Pathology at Pitt, are co-authors on the study.
“This is the first time that gene editing has been used to specifically target cancer fusion genes. It is really exciting because it lays the groundwork for what could become a totally new approach to treating cancer,” explained lead study author Jian-Hua Luo, MD, PhD, professor of pathology at Pitt’s School of Medicine and director of its High Throughput Genome Center.
Fusion genes, which often are associated with cancer, form when two previously separate genes become joined together and produce an abnormal protein that can cause or promote cancer.
Dr. Luo and his team had previously identified a panel of fusion genes responsible for recurrent and aggressive prostate cancer. In a study published earlier this year in the journal Gastroenterology, the team reported that one of these fusion genes, known as MAN2A1-FER, also is found in several other types of cancer, including that of the liver, lungs, and ovaries, and is responsible for rapid tumor growth and invasiveness.
In the current study, the researchers employed the CRISPR-Cas9 genome editing technology to target unique DNA sequences formed because of the gene fusion. The team used viruses to deliver the gene editing tools that cut out the mutated DNA of the fusion gene and replaced it with a gene that leads to death of the cancer cells. Because the fusion gene is present only in cancer cells, not healthy ones, the gene therapy is highly specific. Such an approach could come with significantly fewer side effects when translated to the clinic, which is a major concern with other cancer treatments such as chemotherapy.
To conduct the study, the researchers used mouse models that had received transplants of human prostate and liver cancer cells. Editing the cancer fusion gene resulted in up to 30 percent reduction in tumor size. None of the mice exhibited metastasis and all survived during the 8-week observation period. In contrast, in control mice treated with viruses designed to cut out another fusion gene not present in their tumors, the tumors increased nearly 40-fold in size, metastasis was observed in most animals, and all died before the end of the study.
The new findings suggest a completely new way to combat cancer. “Other types of cancer treatments target the foot soldiers of the army. Our approach is to target the command center, so there is no chance for the enemy’s soldiers to regroup in the battlefield for a comeback,” said Dr. Luo.
Another advantage over traditional cancer treatment is that the new approach is very adaptive. A common problem that renders standard chemotherapies ineffective is that the cancer cells evolve to generate new mutations. Using genome editing, the new mutations could be targeted to continue fighting the disease, Dr. Luo noted.
Illustration: Cancer cell line with CRISPR-based gene therapy delivered via viruses. University of Pittsburgh Medical Center.
AWARDS AND RECOGNITION
Badylak Lab Student Wins First Place in CMU’s CIT Honors Research Poster Competition
 Rinko Maeshima is an undergraduate Research Assistant at the McGowan Institute for Regenerative Medicine and will graduate from Carnegie Mellon University (CMU) majoring in Chemical and Biomedical Engineering. Ms. Maeshima works in the laboratory of McGowan Institute’s Deputy Director Stephen Badylak, DVM, PhD, MD, Professor in the Department of Surgery and Director of the Center for Pre-Clinical Tissue Engineering within the Institute.
Rinko Maeshima is an undergraduate Research Assistant at the McGowan Institute for Regenerative Medicine and will graduate from Carnegie Mellon University (CMU) majoring in Chemical and Biomedical Engineering. Ms. Maeshima works in the laboratory of McGowan Institute’s Deputy Director Stephen Badylak, DVM, PhD, MD, Professor in the Department of Surgery and Director of the Center for Pre-Clinical Tissue Engineering within the Institute.
Recently at CMU’s Meeting of the Minds – Undergraduate Research Symposium, Ms. Maeshima took first place in the CIT Honors Research Poster Competition winning a $500 prize. The title of her poster was “Generation and Evaluation of Porcine Liver Extracellular Matrix as a Tool for Culturing Human Induced Pluripotent (iPSC)-Derived Hepatocytes.”
In Dr. Badylak’s laboratory, Ms. Maeshima works on:
- Investigating how iPS-derived hepatocytes respond in 2D culture to decellularized porcine liver scaffolds through DNA quantification, microscopy and DAPI staining.
- Optimizing the yield of therapeutic proteins from liver ECM scaffolds and analyzing results through RNA extraction, PCR, and quantification
- Physiologically evaluating iPS-derived macrophages through heat map and their response to cytokines, and comparing them to cell line macrophages.
Ms. Maeshima will continue her studies at CMU in the Integrated Master’s program to obtain a Master’s degree in Mechanical Engineering.
Congratulations, Ms. Maeshima!
McGowan Institute for Regenerative Medicine 2017 Top Docs
 The McGowan Institute for Regenerative Medicine applauds its affiliated faculty members who were recently recognized by Pittsburgh Magazine. Each year the magazine commissions Castle Connolly Medical Ltd. to select top doctors on the national and regional levels. The physician-led research team identifies highly skilled, exceptional doctors by evaluating their medical education, training, and hospital appointments, and by surveying area hospital leaders and physicians.
The McGowan Institute for Regenerative Medicine applauds its affiliated faculty members who were recently recognized by Pittsburgh Magazine. Each year the magazine commissions Castle Connolly Medical Ltd. to select top doctors on the national and regional levels. The physician-led research team identifies highly skilled, exceptional doctors by evaluating their medical education, training, and hospital appointments, and by surveying area hospital leaders and physicians.
This year 29 McGowan Institute affiliated faculty were recognized in the May issue of the magazine with 3 colleagues* receiving dual specialty acknowledgment. Congratulations are extended to:
Anesthesiology: Erin Sullivan, MD
Cardiovascular Disease: Dennis McNamara, MD, John Pacella, MD
Critical Care Medicine: Derek Angus, MD, MPH, John Kellum, MD, FACP
Neurological Surgery: David Okonkwo, MD, PhD, Mark Richardson, MD, PhD,* Elizabeth Tyler-Kabara, MD, PhD*
Neurology: Mark Richardson, MD, PhD
Obstetrics and Gynecology: Pamela Moalli, MD, PhD
Orthopedic Surgery: Freddie Fu, MD, MaCalus Hogan, MD, Patrick McMahon, MD, Kurt Weiss, MD
Otolaryngology: Barry Hirsch, MD, Clark Rosen, MD, FACS
Pathology: Anthony Demetris, MD
Pediatric Cardiology: Jacqueline Kreutzer, MD
Pediatric Gastroenterology: Sohail Z. Husain, MD
Pediatric Neurological Surgery: Elizabeth Tyler-Kabara, MD, PhD
Pediatric Surgery: George Gittes, MD, George Mazariegos, MD
Physical Medicine and Rehabilitation: Michael Boninger, MD
Plastic Surgery: Howard Edington, MD,* Ernest Manders, MD, Peter Rubin, MD, Kenneth Shestak, MD
Surgery: Timothy Billiar, MD, Abhinav Humar, MD
Surgical Oncology: Howard Edington, MD
Thoracic Surgery: Thomas Gleason, MD, James Luketich, MD
Congratulations to all!
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#171 –– Dr. George Gittes is is the Benjamin R. Fisher Chair of Pediatric Surgery and Surgeon-in-Chief, Children’s Hospital of Pittsburgh, Director of Surgical Research, Children’s Hospital of Pittsburgh, and Professor of Surgery and Professor of Pediatrics, University of Pittsburgh School of Medicine. Dr. Gittes discusses his research in pancreatic issues as well as his work with the Pediatric Device Initiative.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
PICTURE OF THE MONTH
The Picture of the Month is a compliment to the longstanding features Grant of the Month and Publication of the Month. Each of these features highlights the achievements of McGowan affiliated faculty and their trainees. As we have always welcomed suggestions for grants and publications, please also consider submitting images that can highlight your pioneering work.

Super-resolution image of primary neuron from wild-type mouse cultured for 21 days. Transfected at 7 days in vitro with mitochondrially targeted red fluorescent protein (red) and cytoplasmic green fluorescent protein (green). Image acquired at 100x.
Credits: Anthony Otero, Jason Callio, Charleen Chu lab
PUBLICATION OF THE MONTH
Author: Dhir M, Choudry HA, Holtzman MP, Pingpank JF, Ahrendt SA, Zureikat AH, Hogg ME, Bartlett DL, Zeh HJ, Singhi AD, Bahary N.
Title: Impact of genomic profiling on the treatment and outcomes of patients with advanced gastrointestinal malignancies.
Summary: The impact of genomic profiling on the outcomes of patients with advanced gastrointestinal (GI) malignancies remains unknown. The primary objectives of the study were to investigate the clinical benefit of genomic-guided therapy, defined as complete response (CR), partial response (PR), or stable disease (SD) at 3 months, and its impact on progression-free survival (PFS) in patients with advanced GI malignancies. Clinical and genomic data of all consecutive GI tumor samples from April, 2013 to April, 2016 sequenced by FoundationOne were obtained and analyzed. A total of 101 samples from 97 patients were analyzed. Ninety-eight samples from 95 patients could be amplified making this approach feasible in 97% of the samples. After removing duplicates, 95 samples from 95 patients were included in the further analysis. Median time from specimen collection to reporting was 11 days. Genomic alteration-guided treatment recommendations were considered new and clinically relevant in 38% (36/95) of the patients. Rapid decline in functional status was noted in 25% (9/36) of these patients who could therefore not receive genomic-guided therapy. Genomic-guided therapy was utilized in 13 patients (13.7%) and 7 patients (7.4%) experienced clinical benefit (6 PR and 1 SD). Among these seven patients, median PFS was 10 months with some ongoing durable responses. Genomic profiling-guided therapy can lead to clinical benefit in a subset of patients with advanced GI malignancies. Attempting genomic profiling earlier in the course of treatment prior to functional decline may allow more patients to benefit from these therapies.
Source: Cancer Med. 2017 Jan;6(1):195-206. doi: 10.1002/cam4.992. Epub 2016 Dec 28.
GRANT OF THE MONTH
PI: Anna Balazs
Title: Adaptive Self‐Assembled Systems: Exploiting Multifunctionality for Bottom‐up Large Scale Engineering
Source: Department of Defense MURI Program
Term: 5 years
Amount: $1.5 million per year
