November 2022 | VOL. 21, NO. 11| www.McGowan.pitt.edu
On the Home Stretch?

MIT Technology Review, in an article authored by Senior Reporter-Biomedicine Jessica Hamzelou, highlights the remaining steps to assess the clinical viability of a new therapy that offers the potential to save people with devastating liver diseases who are not eligible for transplants.
The therapy comes from Lygenesis, a McGowan Institute spin-out. Their approach is to inject liver cells from a donor into the lymph nodes of sick recipients, which can give rise to entirely new miniature organs. These mini livers should help to compensate for an existing diseased one. The approach appears to work in preclinical studies. Now the final step is to access if it works in people. Lygenesis is organizing a clinical trial in Boston to answer that important question. The therapy is outlined in the Lygenesis supplied video, available here.
RESOURCES AT THE MCGOWAN INSTITUTE
December Histology Special – Frozen Sections
Let it snow! At the McGowan Histology Core, we are cutting frozen sections and offering 25% off your entire frozen project bill.
We offer a high degree of technical expertise and can accommodate even the more specialized service needs.
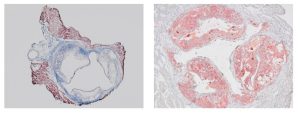
You’ll receive 25% off your frozen project in December when you mention this ad.
Contact Julia at the McGowan Core Histology Lab by email: Hartj5@upmc.edu or call 412-624-5265.
Sample Submission Procedures: In response to COVID-19, we ask that you contact us to schedule a drop off time. When you arrive at the building you can call our laboratory at (412) 624-5365. Someone will meet you in the lobby to collect your samples. When your samples are completed, you will receive an email to schedule a pickup time.
UPCOMING EVENTS
Save the Date! 2023 McGowan Institute Scientific Retreat

The venue for the 2023 Retreat is the University Club, and the dates are March 6 & 7, 2023.
The program committee for the 2023 McGowan Institute Scientific Retreat, under the leadership of Bryan Brown, PhD, has begun to formulate the program and is requesting your suggestions for session topics.
The committee is also seeking to learn of possible interest by individuals in organizing a session. Please submit your program suggestions here.
SCIENTIFIC ADVANCES
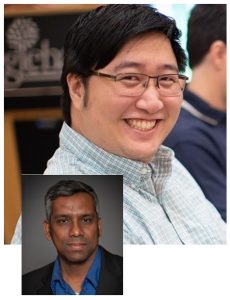
Pitt Study Explains Why Adults’ Hearts Don’t Regenerate

As heart cells mature in mice, the number of communication pathways called nuclear pores dramatically decreases, according to new research from University of Pittsburgh and UPMC scientists. While this might protect the organ from damaging signals, it could also prevent adult heart cells from regenerating, the researchers found.
The study, published in Developmental Cell, suggests that quieting communication between heart cells and their environment protects this organ from harmful signals related to stresses such as high blood pressure, but at the cost of preventing heart cells from receiving signals that promote regeneration.
“This paper provides an explanation for why adult hearts do not regenerate themselves, but newborn mice and human hearts do,” said senior author Bernhard Kühn, MD (pictured top), professor of pediatrics, director of the Pediatric Institute for Heart Regeneration and Therapeutics at Pitt School of Medicine and UPMC Children’s Hospital of Pittsburgh, and an affiliated faculty member of the McGowan Institute for Regenerative Medicine. “These findings are an important advance in fundamental understanding of how the heart develops with age and how it has evolved to cope with stress.”
While skin and many other tissues of the human body retain the ability to repair themselves after injury, the same isn’t true of the heart. During human embryonic and fetal development, heart cells undergo cell division to form the heart muscle. But as heart cells mature in adulthood, they enter a terminal state in which they can no longer divide.
To understand more about how and why heart cells change with age, Dr. Kühn teamed up with fellow Pitt researchers and biomedical imaging experts Yang Liu, PhD, associate professor of medicine and bioengineering, and McGowan Institute faculty member Donna Stolz, PhD (pictured bottom), associate professor of cell biology and pathology and associate director of the Center for Biologic Imaging, to look at nuclear pores. These perforations in the lipid membrane that surround a cell’s DNA regulate the passage of molecules to and from the nucleus.
“The nuclear envelope is an impermeable layer that protects the nucleus like asphalt on a highway,” said Dr. Kühn. “Like manholes in this asphalt, nuclear pores are pathways that allow information to get through the barrier and into the nucleus.”
Using super-resolution microscopy, Dr. Liu visualized and counted the number of nuclear pores in mouse heart cells, or cardiomyocytes. The number of pores decreased by 63% across development, from an average of 1,856 in fetal cells to 1,040 in infant cells to just 678 in adult cells. These findings were validated by Dr. Stolz who used electron microscopy to show that nuclear pore density decreased across heart cell development.
In previous research, Dr. Kühn and his team showed that a gene called Lamin b2, which is highly expressed in newborn mice but declines with age, is important for cardiomyocyte regeneration.
In the new study, they show that blocking expression of Lamin b2 in mice led to a decrease in nuclear pore numbers. Mice with fewer nuclear pores had diminished transport of signaling proteins to the nucleus and decreased gene expression, suggesting that reduced communication with age may drive a decrease in cardiomyocyte regenerative capacity.
“These findings demonstrate that the number of nuclear pores controls information flux into the nucleus,” explained Dr. Kühn. “As heart cells mature and the nuclear pores decrease, less information is getting to the nucleus.”
In response to stress such as high blood pressure, a cardiomyocyte’s nucleus receives signals that modify gene pathways, leading to structural remodeling of the heart. This remodeling is a major cause of heart failure.
The researchers used a mouse model of high blood pressure to understand how nuclear pores contribute to this remodeling process. Mice that were engineered to express fewer nuclear pores showed less modulation of gene pathways involved in harmful cardiac remodeling. These mice also had better heart function and survival than their peers with more nuclear pores.
“We were surprised at the magnitude of the protective effect of having fewer nuclear pores in mice with high blood pressure,” said Dr. Kühn. “However, having fewer communication pathways also limits beneficial signals such as those that promote regeneration.”
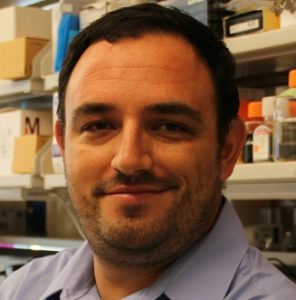
Using 3D Modeling to Stop Cancer’s Spread

Most women diagnosed with metastatic ovarian cancer have a less than 5-year survival rate. Researchers at the University of Pittsburgh Swanson School of Engineering are working to change that.
McGowan Institute for Regenerative Medicine affiliated faculty member Ioannis Zervantonakis, PhD (pictured), assistant professor of bioengineering at Pitt, and his team received $792,000 for four years from the American Cancer Society to understand the biology behind cell interactions that cause ovarian cancer to metastasize to other parts of the body.
To stop ovarian cancer from spreading throughout the abdomen, patients are treated with a combination of surgery and chemotherapy; however, the prognosis is still bleak.
“Because ovarian cancer is diagnosed at a late stage, patients usually don’t respond to chemotherapy,” explained Dr. Zervantonakis. “There is an urgent need to understand how ovarian cancer progresses and develop better bioengineered models that can help researchers discover novel therapeutic targets.”
Ovarian cancer becomes metastatic when tumors are formed by an attachment and growth on mesothelial cells, or cells that cover the outer surface of internal organs in the abdominal cavity. In most cases, these attachments lead to a full invasion of host tissue, significantly lowering the patient’s chance of surviving past treatment.
Cancer cells secrete IGFBP2, a protein associated with a worse prognosis for patients. When IGFBP2 binds to mesothelial cells, it results in activation of the SRC pathway, which supports metastatic progression. The team believes that by targeting this IGFBP2-SRC interaction between cancer cells and mesothelial cells, ovarian cancer metastasis can be stopped.
By developing new three-dimensional models using microfluidic technology (a manipulation of fluid movement at the micron scale), the team will be able to study how production of IGFBP2 by cancer cells impacts mesothelial cell biology and pro-metastatic functions.
“Most of our experiments will be done in 3D microfluidics or mouse models to really give us a good idea of what is actually happening when cells talk to each other through the production of IGFBP2,” said Dorota Jazwinska, a Pitt graduate student leading the experimental work at the Zervantonakis Lab on the project.
Because this project is targeting mesothelial cells in the abdominal cavity, it will eventually be applicable to other types of cancer that colonize abdominal organs.
The grant is expected to begin January 2023. In another project on ovarian cancer metastasis, Dr. Zervantonakis received $160,000 from the Elsa Pardee Foundation in 2020 to study the role of macrophages in metastatic ovarian cancer.
Congratulations, Dr. Zervantonakis!
Illustration: University of Pittsburgh Swanson School of Engineering.
Near-Infrared Spectroscopy Can Provide a Cost-Effective Way to Noninvasively Monitor Intracranial Pressure

An increase in intracranial pressure (ICP) is a dangerous condition that can be caused by brain bleeds, a brain tumor, cerebral edema, traumatic brain injury, and hydrocephalus. ICP monitoring is thus a key aspect of patient care in patients with these disorders. Additionally, ICP measurements are relevant when estimating cerebral perfusion pressure (CPP), an indicator of cerebral autoregulation (CA).
CPP is linked to neuronal function and neurovascular coupling, and CA defines how the brain maintains a constant blood flow. Given these broad implications and applications in clinical decision-making, precise ICP monitoring is a vital patient management tool. While current tools for ICP monitoring are precise, they can cause hemorrhage or infections and are time-consuming.
Although noninvasive alternatives exist, they have limitations such as poor generalizability, low predictive capacity, and a lack of reliability. Thus, diffuse correlation spectroscopy (DCS) and near-infrared spectroscopy (NIRS) are emerging as promising noninvasive solutions. Notably, NIRS has several advantages over other noninvasive methods—low cost, bedside compatibility for long-term and continuous monitoring, along with user independence.
In a new study published in Neurophotonics, researchers at Carnegie Mellon University (CMU)—including McGowan Institute for Regenerative Medicine affiliated faculty member and senior author Jana Kainerstorfer, PhD (pictured)—successfully deployed a NIRS device to continuously monitor hemoglobin concentration changes. The team built on previous research where they estimated ICP from cardiac waveform features measured using DCS, and also identified the correlation between relative changes in oxyhemoglobin concentration and ICP. But how were they able to measure ICP using the NIRS data? First author on the study, Filip Relander, explains, “We developed and trained a random forest (RF) regression algorithm to correlate the morphology of cardiac pulse waveforms obtained through NIRS with intracranial pressure.”
To validate their algorithm, they conducted preliminary tests in a preclinical model. They measured fluctuations in invasive ICP and arterial blood pressure while profiling the changes in hemoglobin concentrations. Following this, they examined the performance of signals derived from the hemoglobin concentration and CBF to accurately verify the precision of their algorithm.
From a proof-of-concept standpoint, the results were very promising. There was a high correlation between the ICP estimated using the RF algorithm and the actual ICP measured using invasive techniques.
“We showed, by validating the findings with invasive ICP data, that the trained RF algorithm applied to NIRS based cardiac waveforms can be used to estimate ICP with a high degree of precision,” said Dr. Kainerstorfer, Associate Professor, Department of Biomedical Engineering and Carnegie Mellon Neuroscience Institute, CMU.
Furthermore, the results indicated that the RF algorithm could interpret waveform features extracted from both NIRS and DCS, highlighting its useability.
The parameters used in the algorithm can be obtained from NIRS measurements, combined with electrocardiograms and mean arterial blood pressure, which are regularly used for clinical evaluation. Thus, if this RF-based platform can produce robust ICP measurements in subsequent human trials, its potential for clinical use would be tremendous. According to Neurophotonics Associate Editor Rickson C. Mesquita, Professor at the University of Campinas, “Assessing ICP noninvasively is of great value for monitoring patients in a critical condition, such as those in the intensive care unit. The future of NIRS in this space is exciting!”
Dr. Partha Roy Lab Member Receives NIH Career Transition Award to Treat Kidney Cancer
David Gau, PhD (pictured top), a lecturer in the University of Pittsburgh Swanson School of Engineering’s Department of Bioengineering, has received a K99/R00 Career Transition Award from the National Institutes of Health (NIH) for his work on clear cell renal cell carcinoma (ccRCC). The award provides $126,047 per year during his two-year fellowship, which proposes a new treatment method for ccRCC.
“More than 75% of renal cell carcinoma is ccRCC and patients with this disease have a five-year survival rate of around 14 percent,” said Dr. Gau, who is a member of the Cell Migration Lab led by McGowan Institute for Regenerative Medicine affiliated faculty member Partha Roy, PhD (pictured bottom). “Our lab wants to investigate the underlying mechanisms associated with this disease so that we can develop more effective treatments.”
ccRCC is characterized by a highly vascular tumor microenvironment within the kidneys and responds well to anti-angiogenic therapies—drugs that block cancer blood vessel growth. Unfortunately, almost all patients develop resistance to these therapies over time. Research has demonstrated that a protein called Profilin1 is linked to human ccRCC and poor clinical outcomes. Dr. Gau’s project, “Profilin as a Novel Target for Vascular Normalization in Renal Cancer,” aims to further develop their previously developed Profilin1 inhibitors as a potential RCC therapy.
“We will also be studying the novel aspects of Profilin1 functionality in endothelial cell biology inside the blood vessels,” he said. “Completion of this project would provide foundational evidence for targeting Profilin1 as a potential treatment for kidney cancer and demonstrate direct impact of Profilin1 on regulation of vessel formation in clear cell renal cell carcinoma.”
The K99/R00 award is the gold standard for training awards for individuals interested in academia and funds two years of mentored training in the K99 phase and three years of independent research in the R00 phase. Dr. Gau hopes to continue his training in contrast-enabled ultrasound and immunobiology as he pivots to the R00 stage of the project.
Congratulations, Dr. Gau!
Illustration: University of Pittsburgh Swanson School of Engineering (Gau)/McGowan Institute for Regenerative Medicine (Roy)
Dr. Seungil Kim Receives Brain Aneurysm Foundation Award

McGowan Institute for Regenerative Medicine affiliated faculty member Seungil Kim, PhD (pictured), is the recipient of the Thomas J. Tinlin Chair of Research Award for $50,000 from the Brain Aneurysm Foundation. Dr. Kim is a Research Assistant Professor in the Department of Surgery at the University of Pittsburgh. He received a PhD in Biomedical Engineering at the University of Manitoba in Canada in 2018.
At Pitt, Dr. Kim is leading and developing projects focusing on developing bioabsorbable embolization systems. As a polymer/biomedical engineer, he designs and develops new materials and devices for better treatment of aneurysms. His father passed away from a stroke, and he hopes he can help patients with a risk of the rupture.
On April 30, 2017, Tom Tinlin’s life was changed forever due to a ruptured brain aneurysm. He was told by one of his doctors that he came as close to dying as one can, without actually doing it. Since that day, Mr. Tinlin learned that three other patients also suffered an aneurysm rupture that same week and went to the same hospital as him, yet he was the only one to survive. Knowing how fortunate he is, Mr. Tinlin and his family have dedicated themselves to raising awareness and funds about this treatable disease. The funds raised not only fund the Thomas J. Tinlin Chair of Research Award, but also go towards brain aneurysm awareness, support, and education. There are 21 Chairs of Research within the Brain Aneurysm Foundation.
Congratulations, Dr. Kim!
Laryngotracheal Reconstruction
Close to 10% of the over 20,000 premature children every year develop airway disorders that often require laryngotracheal reconstruction using cartilage harvested from the rib cage, but this approach is invasive and cannot be applied to younger children, which motivates an urgent need for new, improved technology. The National Heart, Lung, and Blood Institute funded an innovative approach to produce functional cartilage for grafting using decellularized meniscus from a cadaveric donor where selective digestion of tissue components creates channels for recellularization with autologous cell sources obtained by a minimally invasive biopsy. The in vitro and in vivo proposed studies are aimed at defining new, less invasive, and more effective therapeutic options for laryngotracheal reconstruction.
McGowan Institute for Regenerative Medicine affiliated faculty member Riccardo Gottardi, PhD (pictured), is an Assistant Professor of Pediatrics and of Bioengineering at the University of Pennsylvania and the leader of the Bioengineering and Biomaterials Laboratory at the Children’s Hospital of Philadelphia. Dr. Gottardi works closely with clinicians to develop engineering solutions for pediatric airway disorders based on translational tissue engineering and on novel preventative drug delivery approaches with accelerated pathway to the clinic. His lab investigates the basic cellular, molecular, and microbiological mechanisms as well as the genetic aspects of ear, nose, and throat damage and healing, and combines the development of organ-on-chip and animal models of cartilage, vocal folds, and craniofacial tissues to study growth, disease, and repair. He is the principal investigator on the latest 1-year project entitled, “Decellularized Cartilage and Progenitor Cells for Laryngotracheal Reconstruction.” Work began on September 22, 2022.
Newly Issued Patents for McGowan Institute Affiliated Faculty Members

During the months of September and October 2022, the following patents were issued based on research work conducted by McGowan Institute for Regenerative Medicine affiliated faculty members. Their newly issued patents include:
Patent No. 11,433,241
Monitoring and Regulating Physiological States and Functions Via Sensory Neural Inputs to the Spinal Cord
Timothy Burns; Robert Gaunt; Douglas Weber
Patent No. 11,432,731
Novel Ultra-Low Profile Wireless Flow Sensors to Monitor Hemodynamic Alterations in the Vascular System
Young Jae Chun; Brian Jankowitz; Sung Kwon Cho; Yanfei Chen; Woon-Hong Yeo; Connor Howe; Yongkuk Lee
Patent No. 11,433,238
Treatment of Phantom Limb Pain and Diabetic Neuropathy Pain, and Increasing Prosthetic Control by Stimulation of Dorsal Rootlets and Lateral Spinal Cord
Lee Fisher; Douglas Weber; Robert Gaunt
Patent No. 11,445,946
Pedot/CNT Coated Neural Recording Probes for Measurement of Tonic and Phasic Dopamine
Ian Taylor; Xinyan Tracy Cui
Patent No. 11,458,224
Ovarian-Derived Hydrogels for Biomedical and Biotechnology Applications
Michael Buckenmeyer; Bryan Brown; Aleksandar Rajkovic; Yong-Hyun Shin
Patent No. 11,464,479
Method and Apparatus to Detect Lipid Contents in Tissues Using Ultrasound
Kang Kim; Ahmed Mahmoud; Debaditya Dutta
Patent No. 11,471,562
Cartilage Material Having Minimal Hypertrophy and Robust Integration Capacity, And Uses Therefore
Hang Lin; Rocky Tuan; Yanheng Yang
Patent No. D967101
Computing Pointing Device
Rory Cooper; Aaron Anderson; Garrett Grindle; Zachary Kitzmiller Anzelone
Patent number: 11478178
Electronic structures on swollen hydrogels
Christopher J. Bettinger, Haosheng Wu, Congcong Zhu
Patent number: 11472894
Enzyme-assisted ATRP procedures
Krzysztof Matyjaszewski, Alan Enciso Barros, Liye Fu, Alan J. Russell
Congratulations on these successful developments!
Illustration: U.S. Patent and Trademark Office logo.
CPCS Among the Benefits of an Industry Partnership in Pittsburgh

Kris Mamula, writer for the Pittsburgh Post-Gazette, reports that a Massachusetts company is partnering with the University of Pittsburgh and UPMC to advance development of tools used in robotic surgery, reflecting the city’s growing stature in the medical specialty.
Waltham-based Vicarious Surgical Inc., has signed an agreement with Pittsburgh Collaborative Research Education and Technology Advancement in Surgery (CREATES) — a Pitt-UPMC initiative — to enhance devices used in robotic surgery. The pre-revenue company plans to showcase new products at an investors’ conference in December, according to co-founder and CEO Adam Sachs.
Access to another Pitt-UPMC program, the Center for Preclinical Studies at the McGowan Institute for Regenerative Medicine — which is led by Shawn Bengtson, RQAP-GLP — and the expertise of clinical and robotic experts are among the benefits of the partnership in Pittsburgh, the company said. Vicarious, which went public in 2021, reported a net loss of $45.1 million for the third quarter.
Pittsburgh CREATES, started in 2017, is a medical technology innovation center in Oakland that focuses on research, education and developing tech enhancements to surgery. Physician and engineer Umamaheswar Duvvuri, MD, PhD, is the founding director.
Illustration: CPCS logo.
Hoping to Halt Post-Traumatic Osteoarthritis

Every year, nearly 400,000 Americans rupture their anterior cruciate ligament and more than half of them develop post-traumatic osteoarthritis (PTOA) within 15 years. By objectively capturing movement during both natural environment ambulation and physical therapy, research will inform the development of more effective rehabilitation therapies assisted by wearable technology and computer vision/machine learning, promising to halt PTOA and extend the lifespan of natural joints.
McGowan Institute for Regenerative Medicine affiliated faculty member Eni Halilaj, PhD (pictured), Assistant Professor of Mechanical Engineering at Carnegie Mellon University (CMU), with courtesy appointments in Biomedical Engineering and the Robotics Institute at CMU, is the principal investigator on the project entitled, “Digital biomarkers of post-traumatic osteoarthritis: toward precision rehabilitation.” This 5-year project began on September 1, 2022, and is funded by the NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases.
It is widely accepted that failure to restore pre-injury biomechanics after anterior cruciate ligament reconstruction (ACL-R) surgery is one of the key contributing factors to the high prevalence of post-traumatic osteoarthritis (PTOA). Precision rehabilitation, which refers to the delivery of the right feedback to the right patient at the right time, is now a feasible approach
h for PTOA prevention given recent advances in wearable sensing and computer vision technologies. Flexible and unobtrusive skin patches can objectively quantify movement out of the clinic and deliver real-time haptic feedback, while simple videos from smartphones can assess physical therapy quality and deliver corrective visual or auditory feedback. To effectively apply emerging smart-health technologies toward PTOA prevention, the multi-modal and multivariate data produced by these sensors must be distilled to identify digital biomarkers of PTOA that can be targeted with biofeedback therapy in the future.
Accordingly, the central objective of this proposed work is to determine if characteristics of gait extracted from video and wearable sensors (digital biomarkers) can predict longitudinal changes in cartilage microstructure (early PTOA) extracted from quantitative Magnetic Resonance Imaging (qMRI). Our central hypothesis is that future risk of PTOA can be predicted in the first few months after surgery using passively collected data from wearable sensors and video.
This hypothesis is supported by our previous work on pre-arthritic subjects, where we demonstrated that wearable sensing data could predict detrimental changes in cartilage microstructure that are indicative of OA risk. To accomplish the overall objective of this work, physical therapy, natural environment ambulation, and cartilage health will be monitored longitudinally.
Exercise correctness during pre- and post-operative physical therapy will be quantified using computer vision and machine learning algorithms. Out-of-lab movement will be monitored at baseline (3 weeks), 3, and 9 months after surgery with epidermal sensors placed on the thighs and shanks. Quantitative MRI data will be collected at baseline (3 weeks), 3 and 18 months after the surgery. Specifically, we will determine (1) if gait symmetry restoration measured by wearable sensors can predict qMRI changes up to 18 months post-surgery and (2) if physical therapy quality, to the extent that is quantifiable with passive computer vision algorithms, can predict gait symmetry restoration up to 9 months post-surgery.
This work is innovative because it breaks with the current norms of studying the role of biomechanics in PTOA in the laboratory. Instead, we will use wearable sensing, computer vision, and machine learning to generate previously unavailable knowledge on the role of natural environment biomechanics. If successful, this work could enable personalized, technology-assisted rehabilitation—a paradigm shift in clinical care. Additionally, the discovery of new PTOA biomarkers could improve the efficiency of clinical trials for new surgical techniques, while the proposed framework is also extensible to the study and prevention of primary OA, and possibly other orthopaedic conditions.
Congratulations, Dr. Halilaj!
AWARDS AND RECOGNITION
2022 Michael Wells Competition

Michael Wells, Pitt alumnus and successful biotech investor, noted that 2022 marked the 12th year of the competition that he has funded to help accelerate the commercial translation of innovations emerging from University of Pittsburgh labs. In that time, participating teams went on to form 20 spinout companies and have raised $48 million in investment.
This year, EndoDX was named the second-place winners in the 2022 Michael Wells Competition. The team won $15,000. Team members include:
Student: Isabelle Chickanosky, PhD candidate in the Vorp Lab, Department of Bioengineering
Faculty: Timothy Chung, PhD, Research Assistant Professor in the Vorp Lab, Department of Bioengineering; Nicole Donnellan, MD, Associate Professor, Department of Obstetrics, Gynecology and Reproductive Sciences; and David Vorp, PhD (pictured), Associate Dean for Research, Swanson School of Engineering, University of Pittsburgh, the John A. Swanson Professor of Bioengineering, with secondary appointments in the Departments of Cardiothoracic Surgery, Surgery, and the Clinical & Translational Sciences Institute at the University of Pittsburgh, the Co-Director of the Center for Medical Innovation, the Director of the Vascular Bioengineering Laboratory, and an affiliated faculty member of the McGowan Institute for Regenerative Medicine.
Endometriosis is a gynecological disease affecting 10% of women (~200 million) worldwide. These patients often live with chronic pelvic pain (80%) and infertility (50%) but can only seek out diagnosis of this disease via an exploratory surgical laparoscopic procedure. This surgery costs more than $12,000 per procedure, with 60% ending in no endometriosis diagnosis. Prior to the surgery, clinicians who provide these procedures often provide blood tests, ultrasound imaging, or magnetic resonance imaging to identify the presence of this disease, contributing to the average 7-year delay in diagnosis. EndoDx is a machine learning tool to identify risk, presence, and stage of endometriosis in patients non-invasively.
Congratulations, all!
2022 PInCh® Winning Teams Include McGowan Institute Affiliated Faculty Members
The Pitt Innovation Challenge (PInCh®) is an annual program, with 2022 being the 9th year of competition, supported by the Clinical and Translational Science Institute (CTSI) at the University of Pittsburgh. It is designed to generate innovative solutions to challenging health problems by mitigating risk and providing financial and administrative support to move ideas forward. The PInCh program stimulates the translation of novel problem-focused research into the community by giving researchers a venue to be creative, develop new ideas, and work with people beyond their usual sphere of collaborators.
A total of $550,000 was awarded for the 2022 PInCh. Nine awardee teams proposed creative solutions to address important health problems including diagnostics, treatments, interventions, and programs. These solutions, if successfully brought into clinical practice, could significantly improve health outcomes for many and create healthier communities.
After two rounds of pre-selection, the top six teams moved on to the final event where they pitched their ideas to a panel of judges to win up to $115,000. McGowan Institute for Regenerative Medicine affiliated faculty members were members of the three $100,000 Awardees teams and one of the $35,000 Awardees teams. All of the finalists were guaranteed a minimum of $25,000. Three awards were also given to the winners of the virtual PInCh Elevator Pitch Competition.
Bonus Awards for Engineering Good Health were available for PInCh 2022 teams with Pitt faculty leads from both the School of Engineering and Schools of the Health Sciences.
The winning teams with members from the McGowan Institute include:
$100,000 Awardees + $15,000 Bonus Award:
Actin Against ALS (A3). Christi Kolarcik, PhD, and Partha Roy, PhD.
Micro-shield: Abdominal Adhesion Prevention. Steven Little, PhD; Thiagarajan Meyyappan, MD; and, Matthew Rosengart, MD.
Vanish Bioresorbable Stimulator. Trent Emerick, MD, MBA, and Tracy Cui, PhD.
$35,000 Awardees + $15,000 Bonus Award:
Biocarpet. Jonathan Vande Geest, PhD, and John Pacella, MD.
Congratulations, all!
Illustration: PInCH logo.
National Academy of Medicine 2022 Catalyst Awards
The National Academy of Medicine’s (NAM) Healthy Longevity Global Competition is pleased to announce the extension of its international Catalyst Awards through 2025, adding three annual cycles to seed innovative ideas. Focusing on helping accelerate research and entrepreneurism to foster potential breakthroughs in healthy longevity, the Global Competition is a multiyear, multi-phase international competition designed with the aim to help advance bold, novel ideas with the potential to dramatically improve health as people age. The Global Competition consists of three progressive phases during which innovators have the opportunity to compete for increasingly larger awards at the Catalyst, Accelerator, and Grand Prize levels—the latter up to $5 million.
The NAM selected 25 Catalyst Awardees in 2022. McGowan Institute for Regenerative Medicine affiliated faculty member Rosalyn Abbott, PhD (pictured), Assistant Professor in the Departments of Biomedical Engineering and Materials Science and Engineering at Carnegie Mellon University, is one of this year’s honorees. Her project is entitled “Tailoring Tissue Engineering Approaches to the Aging Population.” Catalyst Awards are worth $50,000.
The Global Competition, along with its sister program the Global Roadmap for Healthy Longevity, are part of a larger initiative to fuel a worldwide movement to help improve physical, mental, and social well-being for people as they age, known as the Healthy Longevity Global Grand Challenge. Unique to the Global Competition component in particular is the emphasis on bold, new ideas with the potential for big impact—in disease prevention, mobility, functionality, social connectedness, the biology of aging, and more.
Since its launch in October 2019, the Global Competition has brought together eleven global collaborators representing over 50 countries and territories. The NAM founded the competition and coordinates among a network of global collaborators, each sponsoring a Catalyst Award competition, while also administering a U.S.-based competition. To date, the NAM and its global collaborators have issued more than $23.5 million in award funding to nearly 430 Catalyst and 13 Accelerator Awardees worldwide.
Congratulations, Dr. Abbott!
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#239 –– Mr. Shawn Bengtson discusses his work in Quality Management Systems and how it differs from Good Lab Practices.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
PUBLICATION OF THE MONTH
Author: Lu Han, Jocelyn D Mich-Basso, Yao Li, Niyatie Ammanamanchi, Jianquan Xu, Anita P Bargaje, Honghai Liu, Liwen Wu, Jong-Hyeon Jeong, Jonathan Franks, Donna B Stolz, Yijen L Wu, Dhivyaa Rajasundaram, Yang Liu, Bernhard Kühn
Title: Changes in nuclear pore numbers control nuclear import and stress response of mouse hearts
Summary: Nuclear pores are essential for nuclear-cytoplasmic transport. Whether and how cells change nuclear pores to alter nuclear transport and cellular function is unknown. Here, we show that rat heart muscle cells (cardiomyocytes) undergo a 63% decrease in nuclear pore numbers during maturation, and this changes their responses to extracellular signals. The maturation-associated decline in nuclear pore numbers is associated with lower nuclear import of signaling proteins such as mitogen-activated protein kinase (MAPK). Experimental reduction of nuclear pore numbers decreased nuclear import of signaling proteins, resulting in decreased expression of immediate-early genes. In a mouse model of high blood pressure, reduction of nuclear pore numbers improved adverse heart remodeling and reduced progression to lethal heart failure. The decrease in nuclear pore numbers in cardiomyocyte maturation and resulting functional changes demonstrate how terminally differentiated cells permanently alter their handling of information flux across the nuclear envelope and, with that, their behavior.
Source: Dev Cell. 2022 Oct 24;57(20):2397-2411.e9.
GRANT OF THE MONTH
PI: Charleen Chu
Title: Protein homeostasis in a frontotemporal dementia iPSC model
Description: Maintaining protein homeostasis is a particular challenge for neurons, in which a high demand for protein synthesis, folding and transport represents a constant source of stress. Evidence of protein mishandling is observed in nearly all neurodegenerative diseases including the AD-related dementias (ADRD). The AAA- ATPase valosin-containing protein (VCP) plays a central role in maintaining multiple aspects of protein homeostasis. Mutations in VCP have been linked to several forms of frontotemporal lobar degeneration with or without concurrent motor dysfunction and musculoskeletal disease. Yet there is limited understanding of how these mutations affect different aspects of VCP function in neurons. The VCP-T262A mutation causes familial frontotemporal dementia with aphasia and parkinsonism. Preliminary studies in primary neurons transfected with VCP-T262A reveal deficits in dendritic arborization, and patient fibroblasts bearing the endogenous mutation exhibit disrupted secretory function. Reagents to create human neurons and other relevant cell types bearing the endogenous VCP-T262A mutation are critically needed to study pathophysiological mechanisms of disease. In this exploratory project, we will create isogenic pairs of iPSC lines expressing T262A vs. wild type VCP. We will differentiate to cortical neurons to study the effects of this mutation upon ER stress, autophagy and Golgi markers compared to iPSC-derived cells with a mutation in a different VCP functional domain. Our long-range goals are to understand how alterations in VCP contribute to synaptic loss so that this mechanistic understanding can be translated into new therapeutic approaches.
Source: National Institute on Aging
Term: August 01, 2022 – July 31, 2024
Amount: $434,890


