Garrett Coyan, MD, sees many patients each week, from children to the elderly, to check on their replacement heart valves.
“We have to counsel patients every day on which current technology is right for them, including what medicine they need to take and what limitations they have for their lifestyle,” said Dr. Coyan, a resident in the University of Pittsburgh’s six-year integrated cardiothoracic surgery residency program and a team member in the lab of McGowan Institute for Regenerative Medicine director, William Wagner, PhD. “It can be hard to do sometimes.”
Heart valve disease affects over 2.5% of the US population, resulting in the need for over 150,000 heart valve replacements each year—and the need is only growing. Current mechanical and bio-prosthetic replacement valves have drawbacks, however. They require a lifelong commitment to a strict blood-thinning medicine regimen, aren’t very durable, and don’t allow for growth when implanted in children.
“There’s a serious need for valves that will last longer,” said Dr. Coyan. “For children, you’re basically setting them up for several operations in their lifetime, because you don’t have an option that can last for the entirety of their adolescence. They might need up to four operations to get to adulthood.”
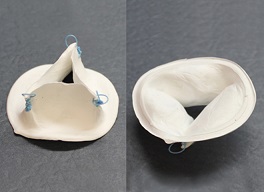
Seeing this trend, Dr. Coyan and a team of researchers at the McGowan Institute work to create an engineered, scaffold-based heart valve replacement that relies on internal tissue growth. In other words, the device, called OneValve, recruits the patient’s cells to help it grow within the patient, meaning anticoagulation therapy and costly reoperations wouldn’t be necessary.
“We use biopolymer materials that degrade over time, and these materials create a mesh that works as a valve immediately,” Dr. Coyan said. “But the cool thing is, over time, the patient’s own cells will invade that mesh and grow into it. After about a year to a year-and-a-half, the patient’s cells have created their own heart valve in its place.”
The mesh provides an organic blueprint for cells to latch onto and reproduce to recreate the natural valve that current replacement valves can’t achieve.
“Mechanical valves and bioprosthetics are simply not designed to perform those kinds of tasks,” said Antonio D’Amore, PhD, research assistant professor in the departments of surgery and bioengineering at Pitt and also a team member in the Wagner Lab. “Cells can’t attach to those valves and treat them as foreign objects. This mesh acts like a sponge for those cells.”
Dr. D’Amore is another lead investigator for OneValve, as well as a principal investigator and head of the cardiac tissue engineering program, Fondazione RiMED, an international partnership between the Italian government, the University of Pittsburgh, and the University of Pittsburgh Medical Center.
The OneValve team’s prototype proved to be successful in 24-hour porcine studies. The team next wants to test the device for a longer period of time, about several months, and move OneValve more toward clinical trials and commercialization.
And, as winners of the 2019 Pitt Innovation Challenge hosted by Pitt’s Clinical and Translational Science Institute, that next step is very near.
“We’re excited about it. We’re happy to have won the competition and will use the resources to move things along,” said Dr. Wagner, Distinguished Professor in the departments of surgery, bioengineering and chemical engineering at Pitt, and a third lead investigator for OneValve.
The team has also been working with Pitt’s Innovation Institute to move OneValve more toward commercialization.
Illustration: The OneValve device shown here recruits a patient’s own cells to the heart valve, then degrades over time, coaxing a natural replacement heart valve into being. The blue sutures pictured anchor the device to the right ventricle of the heart. (Courtesy of OneValve.)
Read more…
