January 2022 | VOL. 21, NO. 1| www.McGowan.pitt.edu
Dr. David Kaczorowski Member of Surgical Team on Historic First Successful Transplant of Porcine Heart into Adult Human with End-Stage Heart Disease
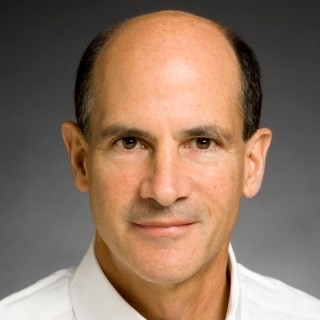
In a first-of-its-kind surgery, a 57-year-old patient with terminal heart disease received a successful transplant of a genetically modified pig heart and is still doing well three days later. It was the only currently available option for the patient. The historic surgery was conducted by University of Maryland School of Medicine (UMSOM) faculty at the University of Maryland Medical Center (UMMC), together known as the University of Maryland Medicine. Bartley P. Griffith, MD (pictured middle), surgically transplanted the pig heart into the patient.
Today, Dr. Griffith is the Thomas E. and Alice Marie Hales Distinguished Professor in Transplant Surgery at UMSOM and Director of the Cardiac Transplant Program at UMMC. Prior to this appointment, Dr. Griffith served as the chief of cardiothoracic surgery at the University of Pittsburgh School of Medicine (UPMC). He was also the founder of The McGowan Center for Artificial Organ Development which was established in 1992 from a $1 million donation from William G. McGowan, founder and chairman of MCI Communications. The McGowan Institute for Regenerative Medicine was formed in 2001 by consolidating the artificial organ and medical device research of the faculty affiliated with the McGowan Center with research related to tissue engineering and cell-based therapies. The McGowan Institute works on tissue and organ insufficiency through tissue engineering, cell-based therapies, and medical devices and artificial organs, with an emphasis on translating the research findings of McGowan Institute affiliated faculty into clinical use.
This organ transplant demonstrated for the first time that a genetically modified animal heart can function like a human heart without immediate rejection by the body. The patient, David Bennett, a Maryland resident, is being carefully monitored over the next days and weeks to determine whether the transplant provides lifesaving benefits. He had been deemed ineligible for a conventional heart transplant at UMMC as well as at several other leading transplant centers that reviewed his medical records.
“It was either die or do this transplant. I want to live. I know it’s a shot in the dark, but it’s my last choice,” said Mr. Bennett, the patient, a day before the surgery was conducted. He had been hospitalized and bedridden for the past few months. “I look forward to getting out of bed after I recover.”
The U.S. Food and Drug Administration granted emergency authorization for the surgery on New Year’s Eve through its expanded access (compassionate use) provision. It is used when an experimental medical product, in this case the genetically modified pig’s heart, is the only option available for a patient faced with a serious or life-threatening medical condition. The authorization to proceed was granted in the hope of saving the patient’s life.
“This was a breakthrough surgery and brings us one step closer to solving the organ shortage crisis. There are simply not enough donor human hearts available to meet the long list of potential recipients,” said Dr. Griffith. “We are proceeding cautiously, but we are also optimistic that this first-in-the-world surgery will provide an important new option for patients in the future.”
Considered one of the world’s foremost experts on transplanting animal organs, known as xenotransplantation, Muhammad M. Mohiuddin, MD (pictured bottom), Professor of Surgery at UMSOM, joined the UMSOM faculty five years ago and established the Cardiac Xenotransplantation Program with Dr. Griffith. Dr. Mohiuddin serves as the program’s Scientific/Program Director and Dr. Griffith as its Clinical Director.
“This is the culmination of years of highly complicated research to hone this technique in animals with survival times that have reached beyond nine months. The FDA used our data and data on the experimental pig to authorize the transplant in an end-stage heart disease patient who had no other treatment options,” said Dr. Mohiuddin. “The successful procedure provided valuable information to help the medical community improve this potentially life-saving method in future patients.”
About 110,000 Americans are currently waiting for an organ transplant, and more than 6,000 patients die each year before getting one, according to the federal government’s organdonor.gov. Xenotransplantation could potentially save thousands of lives but does carry a unique set of risks, including the possibility of triggering a dangerous immune response. These responses can trigger an immediate rejection of the organ with a potentially deadly outcome to the patient.
Before consenting to receive the transplant, Mr. Bennett, the patient, was fully informed of the procedure’s risks, and that the procedure was experimental with unknown risks and benefits. He had been admitted to the hospital more than six weeks earlier with life-threatening arrhythmia and was connected to a heart-lung bypass machine, called extracorporeal membrane oxygenation (ECMO), to remain alive. In addition to not qualifying to be on the transplant list, he was also deemed ineligible for an artificial heart pump due to his arrhythmia.
Revivicor, a regenerative medicine company based in Blacksburg, VA, provided the genetically modified pig to the xenotransplantation laboratory at UMSOM. On the morning of the transplant surgery, the surgical team, led by Dr. Griffith and Dr. Mohiuddin, removed the pig’s heart and placed it in the XVIVO Heart Box, perfusion device, a machine that keeps the heart preserved until surgery. McGowan Institute for Regenerative Medicine affiliated faculty member David Kaczorowski, MD (pictured top), Surgical Director of the Advanced Heart Failure Center of UPMC Heart and Vascular Institute and an Associate Professor of Cardiothoracic Surgery, Department of Cardiothoracic Surgery, University of Pittsburgh, was a member of this landmark surgical transplant team. Previously, he worked at the University of Maryland with Dr. Griffith and Dr. Mohiuddin to perfect the pig-to-baboon heart transplants.
“This is an important step forward in medicine,” said Dr. Kaczorowski, who helped procure the heart from the donor pig. While it will likely be several years before pig organs are routinely used in humans, he said, this is a huge step in that direction. “This is the medical equivalent of landing on the moon,” he said.
The physician-scientists also used a new drug along with conventional anti-rejection drugs, which are designed to suppress the immune system and prevent the body from rejecting the foreign organ. The new drug used is an experimental compound made by Kiniksa Pharmaceuticals.
Organs from genetically modified pigs have been the focus of much of the research in xenotransplantation, in part because of physiologic similarities between pigs, human, and nonhuman primates. UMSOM received $15.7 million sponsored research grant to evaluate Revivicor genetically modified pig UHearts™ in baboon studies.
Three genes—responsible for rapid antibody-mediated rejection of pig organs by humans—were “knocked out” in the donor pig. Six human genes responsible for immune acceptance of the pig heart were inserted into the genome. Lastly, one additional gene in the pig was knocked out to prevent excessive growth of the pig heart tissue, which totaled 10 unique gene edits made in the donor pig.
Illustration: McGowan Institute for Regenerative Medicine (Kaczorowski)/University of Maryland Medical Center (Griffith/Mohiuddin)
RESOURCES AT THE MCGOWAN INSTITUTE
February Histology Special – Cardiac Samples
The Histology Core wants to be your Valentine this month with big saving that will warm your heart.
Bring your cardiac tissue to the McGowan Histology Core and receive 25% off your entire order in the month of February when you mention this ad.
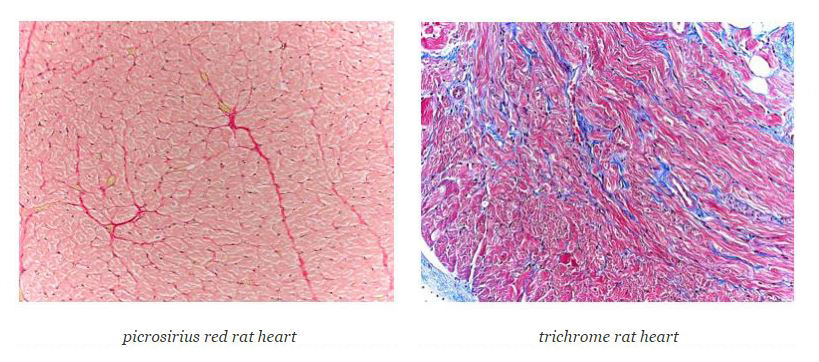
You’ll receive 25% off cardiac samples in February when you mention this ad.
Contact Julia at the McGowan Core Histology Lab by email: Hartj5@upmc.edu or call 412-624-5265.
New Sample Submission Procedures: In response to COVID-19, we ask that you contact us to schedule a drop off time. When you arrive at the building you can call our laboratory at (412) 624-5365. Someone will meet you in the lobby to collect your samples. When your samples are completed, you will receive an email to schedule a pickup time.
Save the Date-2022 McGowan Institute Scientific Retreat
 Now Open for the 2022 McGowan Institute Scientific Retreat
Now Open for the 2022 McGowan Institute Scientific Retreat
The 21st Annual McGowan Institute for Regenerative Medicine Virtual Scientific Retreat will take place on March 7-8, 2022.
The poster session will be held on March 7th.
Under the leadership of McGowan Institute for Regenerative Medicine faculty member Bryan Brown, PhD, associate professor, Department of Bioengineering the program committee is planning an exciting group of speakers and topics.
Mark the dates on your calendars. Additional 2022 Retreat details and news will be available here.
Call for Abstracts – 2022 Military Health System Research Symposium
 The 2022 Military Health System Research Symposium (MHSRS) Call for Abstracts is now open and runs until 16 February 2022. We WILL NOT accept abstract submissions after 16 February, so please plan accordingly.
The 2022 Military Health System Research Symposium (MHSRS) Call for Abstracts is now open and runs until 16 February 2022. We WILL NOT accept abstract submissions after 16 February, so please plan accordingly.
The MHSRS is the Department of Defense’s premier scientific meeting. It provides a collaborative environment for military medical care providers with deployment experience, DoD scientists, academia, and industry to meet and exchange information on the unique medical needs of the Warfighter.
The theme of the 2022 MHSRS is “Optimizing Readiness…The Power of Military Medical Research”. The meeting will have four presentation focus areas: Warfighter Medical Readiness, Expeditionary Medicine, Warfighter Performance, and Return to Duty. In addition, there will be breakout sessions dedicated to DoD-sponsored SARS CoV-2 (COVID-19) related research.
Go to the MHSRS website to review the titles and descriptions of the 2022 scientific breakout sessions and to submit an abstract.
The MHSRS website is a password enabled site.
(1) Army MEDCOM and DHA CAC Users: Signing in with a CAC is the most secure/desirable method since it uses two-factor authentication.
Go to the MHSRS Portal (Click ‘Sign In with CAC’). If you have trouble accessing with your CAC, please register for a member account.
(2) All Others must have a username and password to access the site and to submit an abstract. If you have forgotten your previously issued username and password, email for assistance. DO NOT re-register. If you have never registered on the MHSRS website (new abstract submitter), go to the MHSRS Website Registration Page to register for a new member account and receive username and password.
As of this time, we are projecting the 2022 MHSRS to be an in-person meeting. Meeting Approval is pending. The date and location are pending. This information will be posted on the MHSRS website and communicated via a mass e-mail to those registered on the MHSRS website when it is available.
SCIENTIFIC ADVANCES
Traumatic Injury Response Characterized for First Time on Cellular Level
The first-ever, in-depth characterization of the body’s response to traumatic injury was published in Cell Reports Medicine by University of Pittsburgh School of Medicine physician-scientists. The results of their multiomics analysis—which spanned thousands of circulating molecules—offers an opportunity to refine personalized approaches to trauma management in the most severely injured patients.
“We are finally seeing a comprehensive picture of how the human body responds to systemic injury, when a person is taken from a state of relative health and pushed into an almost lethal state within microseconds,” said main corresponding author Timothy Billiar, MD, distinguished professor of surgery at Pitt, chief scientific officer for UPMC, and affiliated faculty member of the McGowan Institute for Regenerative Medicine. “We’ve never quite known how different components of the human injury response fit together, so this is a trauma researcher’s dream come true.”
Other McGowan Institute affiliated faculty members involved in this study include:
- Yoram Vodovotz, PhD, professor in the Department of Surgery with secondary appointments in the Department of Computational & Systems Biology, the Department of Bioengineering, the Department of Immunology, the Department of Communication Science and Disorders (of the School of Health and Rehabilitation Science), and the Clinical and Translational Science Institute, and the director of the Center for Inflammation and Regeneration Modeling at the McGowan Institute
- David Okonkwo, MD, PhD, professor of neurological surgery, director of the Neurotrauma Clinical Trials Center, director of Neurotrauma and of the Scoliosis and Spinal Deformity Program at UPMC, and clinical director of the Brain Trauma Research Center
- Rami Namas, MD, Assistant Professor, Department of Surgery, University of Pittsburgh
When emergency medical response teams get called into action, they know that time is of the essence. The arsenal of therapeutic tools available to trauma responders is limited, and, for patients who suffered massive injury from a car crash or a fall, every lost second can mean the difference between life and death.
Prehospital care therapies, such as thawed blood plasma administered even before the patient makes it to the hospital, can be astonishingly successful in increasing the odds of survival. More than three years ago, a clinical trial led by Pitt School of Medicine clinicians showed that trauma patients at risk of hemorrhagic shock who received two units of blood plasma during air medical transport were 10% more likely to survive than those who did not.
“The 10% reduction in mortality borders on unprecedented,” said clinical trial lead and co-senior author Jason Sperry, MD, MPH, professor in the departments of surgery and critical care medicine in Pitt’s School of Medicine. “In the decades of research on trauma interventions, we have never seen such a big impact from such a small intervention. The benefits of giving plasma to trauma patients during air transport are extraordinary and practice-changing.”
But not every trauma patient benefits from early plasma administration. To ensure that therapeutic interventions are distributed in a way that maximizes the benefits and minimizes the waste of precious resources—especially during the ongoing plasma shortage further worsened by the pandemic—there is a strong need to identify those most likely to respond favorably to plasma early after injury.
Such an identification—which mirrors personalized approaches frequently used in the field of oncology—has never been achieved for trauma before.
“Despite how ubiquitous the problem is, the current therapies available for trauma patients are blunt instruments,” said co-senior author Matthew D. Neal, MD, the Roberta G. Simmons associate professor of surgery at Pitt. “The complexity of perturbations that happen to a human body within seconds after injury is not something that we’ve ever understood before.”
By analyzing thousands of circulating proteins and lipids, along with byproducts of cell metabolism and biomarkers of vessel injury, the clinicians discovered that human traumatic injury response could be classified into two “endotypes.” They also found that only endotype 2 patients who also suffered traumatic brain injury benefitted from the infusion of thawed plasma—nearly 70% of those patients were alive 30 days after the injury, compared to 25% of endotype 1 patients.
The group also identified a single blood biomarker—a nerve cell enzyme called ubiquitin carboxyl-terminal esterase L1, or UCHL1, that is predictive of a favorable response to thawed plasma therapy.
Understanding the universe of interactions between molecules released into the bloodstream after traumatic injury has been a dream of health scientists for decades. The progress in technologies that allow for high-throughput identification of circulating biomarkers, combined with newly available computational techniques, have finally made it possible to peek behind the curtain and uncover part of the complexity behind the body’s response to sudden and severe injury.
Translating these insights into clinical practice is the next great race, doctors say. Point-of-care diagnostics that allow physicians to quickly test for a panel of blood biomarkers already exist and might be available more widely in the next five years, with this recent study guiding clinical action based on the results.
Leveraging Space to Advance Stem Cell Science and Medicine

The secret to producing large batches of stem cells more efficiently may lie in the near-zero gravity conditions of space. Scientists at Cedars-Sinai have found that microgravity has the potential to contribute to life-saving advances on Earth by facilitating the rapid mass production of stem cells.
A new paper, led by Cedars Sinai and published in the peer-review journal Stem Cell Reports, highlights key opportunities discussed during the 2020 Biomanufacturing in Space Symposium to expand the manufacture of stem cells in space. McGowan Institute for Regenerative Medicine faculty members William Wagner, PhD, Director of the McGowan Institute and Distinguished Professor of Surgery, Chemical Engineering, and Bioengineering at the University of Pittsburgh, and Patrick Cantini, Strategy and Business Development Officer at the McGowan Institute, are co-authors of the study.
Biomanufacturing — a type of stem cell production that uses biological materials such as microbes to produce substances and biomaterials suitable for use in preclinical, clinical, and therapeutic applications — can be more productive in microgravity conditions.
“We are finding that spaceflight and microgravity is a desirable place for biomanufacturing because it confers a number of very special properties to biological tissues and biological processes that can help mass produce cells or other products in a way that you wouldn’t be able to do on Earth,” said stem cell biologist Arun Sharma, PhD, research scientist and head of a new research laboratory in the Cedars-Sinai Board of Governors Regenerative Medicine Institute, Smidt Heart Institute and Department of Biomedical Sciences.
“The last two decades have seen remarkable advances in regenerative medicine and exponential advancement in space technologies enabling new opportunities to access and commercialize space,” he said.
Attendees at the virtual space symposium in December identified more than 50 potential commercial opportunities for conducting biomanufacturing work in space, according to the Cedars-Sinai paper. The most promising fell into three categories: disease modeling, biofabrication, and stem-cell-derived products.
The first, disease modeling, is used by scientists to study diseases and possible treatments by replicating full-function structures — whether using stem cells, organoids (miniature 3D structures grown from human stem cells that resemble human tissue), or other tissues.
Investigators have found that once the body is exposed to low-gravity conditions for extended periods of time, it experiences accelerated bone loss and aging. By developing disease models based on this accelerated aging process, research scientists can better understand the mechanisms of the aging process and disease progression.
“Not only can this work help astronauts, but it can also lead to us manufacturing bone constructs or skeletal muscle constructs that could be applied to diseases like osteoporosis and other forms of accelerated bone aging and muscle wasting that people experience on Earth,” said Dr. Sharma, who is the corresponding author of the paper.
Another highly discussed topic at the symposium was biofabrication, which uses manufacturing processes to produce materials like tissues and organs. 3D printing is one of the core biofabrication technologies.
A major issue with producing these materials on Earth involves gravity-induced density, which makes it hard for cells to expand and grow. With the absence of gravity and density in space, scientists are hopeful that they can use 3D printing to print unique shapes and products, like organoids or cardiac tissues, in a way that can’t be replicated on Earth.
The third category has to do with the production of stem cells and understanding how some of their fundamental properties are influenced by microgravity. Some of these properties include potency, or the ability of a stem cell to renew itself, and differentiation, the ability for stem cells to turn into other cell types.
Understanding some of the effects of spaceflight on stem cells can potentially lead to better ways to manufacture large numbers of cells in the absence of gravity. Scientists from Cedars-Sinai will be sending stem cells into space early next year, in conjunction with NASA and a private contractor, Space Tango, to test whether it is possible to produce large batches in a low gravity environment.
“While we are still in the exploratory phase of some of this research, this is no longer in the realm of science fiction,” Dr. Sharma said. “Within the next five years we may see a scenario where we find cells or tissues that can be made in a way that is simply not possible here on Earth. And I think that’s extremely exciting.”
Measuring Tiny Eye Movements Can Help Identify Vision Impairments After Concussions
For up to 3 million Americans each year, what was supposed to be a fun day at the ski slopes, at a playground or on a football field quickly takes a turn for the worse. While simple steps – such as wearing a helmet – can prevent serious head injury resulting from a sudden high-impact fall or a blow to the head, those measures are less effective at preventing concussions.
In collaboration with the UPMC Concussion group, researchers from the University of Pittsburgh Department of Ophthalmology discovered that recording and analyzing patterns of fixational saccades – tiny involuntary eye movements that help maintain the gaze on a stationary object or location – can be used to develop fast, non-invasive, and reliable tools to identify vision impairment following concussion, which sometimes goes undiagnosed. The report was published recently in the Journal of Vision.
“Our group was the first to precisely evaluate fixational eye movements in patients following a concussion,” said senior author Ethan Rossi, PhD, assistant professor of ophthalmology at Pitt. Dr. Rossi is also an affiliated faculty member of the McGowan Institute for Regenerative Medicine.
Concussion is a mild traumatic brain injury. People suffering from a concussion often feel dizzy, experience headaches and can develop vision problems. Identifying all symptoms and impairments requires a careful and comprehensive assessment – and the success of a patient’s recovery hinges on it.
Although there is no single treatment for all concussions, treatments that target anxiety and headache, and that are aimed to restore brain function, balance, and vision, can accelerate recovery. Still, the tools for evaluating vision impairments following concussions are limited, which can lead to missed opportunities for more effective treatments.
To address that issue, the researchers tested whether concussion affects small involuntary eye movements, and whether that measurement can be used to assess vision impairments in patients. The scientists found that young adults and adolescents who were tested several days after their concussion had greater fixational saccade amplitude – meaning that their involuntary eye movements were larger and less precisely controlled than normal — when trying to focus on the center of an object than those without concussion. The finding points at the possibility of using that parameter, and potentially other metrics based on eye movements, to reliably assess visual dysfunction in people with suspected concussion.
And the technology to measure the saccades already exists. The researchers collaborated with a biotechnology startup from Boston, led by vision science expert Christy Sheehy, PhD, that developed and patented an eye-tracking device that’s capable of recording and analyzing eye movements with higher precision than existing commercial devices.
“This technology has the potential to add objectivity to our ability to identify visual impairment in patients following concussion that might otherwise go undetected using current clinical evaluations,” said co-author Anthony Kontos, PhD, director of the UPMC Sports Medicine Concussion Program. “Using eye movement analysis can complement current clinical assessments and provide a more objective, measurable outcome to identify and track patients’ recovery.”
Possible Stroke Therapy Advances with Development of a Cell Tracking Tool

Early results with injection of ECM hydrogel into brain tissue cavities formed by stroke have shown potentially promising therapeutic outcomes. Extracellular matrix (ECM) hydrogel implantation into a stroke-induced tissue cavity invokes a robust cellular immune response. However, the spatio-temporal dynamics of immune cell infiltration into peri-infarct brain tissues versus the ECM-bioscaffold have remained poorly understood. In a recently published report entitled “Mapping the acute time course of immune cell infiltration into an ECM hydrogel in a rat model of stroke using 19F MRI”; Biomaterials; online 25 January 2022, 121386 by McGowan faculty members Michel Modo, PhD and Steven Badylak, DVM, PhD, MD and colleagues, the authors tagged peripheral immune cells using perfluorocarbon (PFC) nanoemulsions that afford their visualization by 19F magnetic resonance imaging (MRI). Prior to ECM hydrogel implantation, only blood vessels could be detected using 19F MRI. Using “time-lapse” 19F MRI, the study established the infiltration of immune cells into the peri-infarct area occurs 5–6 hours post-ECM implantation. Immune cells also infiltrated through the stump of the MCA, as well as a hydrogel bridge that formed between the tissue cavity and the burr hole in the skull.
Tissue-based migration into the bioscaffold was observed between 9-12 hours with a peak signal measured between 12-18 hours post-implantation. Fluorescence-activated cell sorting of circulating immune cells revealed that 9% of cells were labeled with PFC nanoemulsions, of which the vast majority were neutrophils (40%) or monocytes (48%). Histology at 24 h post-implantation, in contrast, indicated that macrophages (35%) were more numerous in the peri-infarct area than neutrophils (11%), whereas the vast majority of immune cells within the ECM hydrogel were neutrophils (66%). Only a small fraction (12%) of immune cells did not contain PFC nanoemulsions, indicating a low type II error for 19F MRI. 19F MRI hence provides a unique tool to improve our understanding of the spatio-temporal dynamics of immune cells invading bioscaffolds and effecting biodegradation.
Mapping the Cell Specific DNA Damage-Induced Molecular and Bioelectrical Responses in the 3D Cardiac Unit

Increased DNA damage and DNA damage response (DDR) activation is well-documented in cardiovascular disease (CVD) and heart failure in humans, but no current treatment strategies exist to target this population. By applying cutting-edge optical, biological, and bioelectrical tools, McGowan Institute for Regenerative Medicine affiliated faculty member Tzahi Cohen-Karni, PhD, Associate Professor in the Department of Biomedical Engineering at Carnegie Mellon University, and his team will map cardiac tissue cell-cell communication and electrophysiology in response to stochastic endogenous DNA damage. Deeper understanding of the regulatory network that mediates the genotoxic stress response in the cardiac tissue will suggest preventive strategies and therapeutic interventions to reduce public health burden.
This project, entitled “Mapping the cell specific DNA damage-induced molecular and bioelectrical responses in the 3D cardiac unit,” will run for 5 years. It is funded by the National Heart, Lung, and Blood Institute.
The project abstract follows:
This project will test the hypothesis that DNA damage in cardiomyocytes activates p53 leading to mitochondrial alterations and secretion of paracrine factors that drive heart failure. The premise for this has been established from our preliminary data and from the work of others. First, DNA damage and activated DNA damage response (DDR) have been observed in cardiovascular disease (CVD) in humans. Second, studies also show evidence that multiple cell types in the cardiac unit, including cardiomyocytes (CM) and cardiac fibroblasts (CF) display markers of DNA damage and cellular senescence in several disease pathologies. Third, we have recently identified that nuclear DNA damage drives dilated cardiomyopathy. Specifically, cardiomyocyte-depletion of the DNA repair endonuclease, ERCC1-XPF in mice, upregulates the DNA damage response gene, p53, and leads to irregular mitochondrial cristae, accumulation of lipids and increased oxidative stress. Additionally, there is an increase in several cardiac failure and senescence associated markers. However, the exact molecular underpinnings and cell-specificity of these DNA damage-induced changes is poorly understood. One barrier to addressing this question in vivo has been lack of appropriate tools, where DNA damage can be introduced in only one cell type (e.g., CM) and its effect on CF and cardiac function can be investigated. Additionally, 2D cell culture and co-culture systems fall short, as they cannot reproduce tissue dynamics present in a cardiac unit. Herein, we have developed several tools which enable the study of cell-cell communication of 3D multicellular system. Specific Aim 1 will map the molecular, functional, and architectural changes upon loss of ERCC1 in CM. In this aim, we will test the mechanistic role of p53 and reactive oxygen species on a number of cellular and mitochondrial parameters, as well as cardiomyocyte electrophysiology. Specific Aim 2 will test whether stochastic, spontaneous DNA damage in the CM or CF drives cardiac electromechanical dysfunction in a cell autonomous or cell non-autonomous manner through a paracrine effect on neighboring cells. Here, we will analyze the pathological secretome upon genotoxic stress, as well as test the role of eliminating senescent cells on cardiac health. This work is technically innovative as it uses a number of unique tools including concomitant optical and bioelectrical measurements in 3D cardiac organoids. These contributions will be significant because DNA damage is unavoidable and intimately linked to cardiac health and disease. Our team is uniquely qualified to perform this work, with expertise in DNA damage/repair, cellular senescence, nanofabrication, human iPSC-derived cardiac tissue engineering, and data science. This analysis, we believe, will increase our fundamental understanding of the connection between DNA damage and heart disease and potentially pave the way for new treatment strategies.
Blood from Marathoner Mice Boosts Brain Function in Their Couch-Potato Counterparts
Physical exercise is great for a mouse’s brain, and for yours. Numerous studies conducted in mice, humans and laboratory glassware have made this clear. Now, a new study shows it’s possible to transfer the brain benefits enjoyed by marathon-running mice to their couch-potato peers.
Stanford School of Medicine researchers—including McGowan Institute for Regenerative Medicine affiliated faculty member Thomas Rando, MD, PhD, the Director of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at the University of California, Los Angeles (formerly, a Professor, Department of Neurology and Neurological Sciences, Stanford University School of Medicine)—have shown that blood from young adult mice that are getting lots of exercise benefits the brains of same-aged, sedentary mice. A single protein in the blood of exercising mice seems largely responsible for that benefit.
The discovery could open the door to treatments that — by taming brain inflammation in people who don’t get much exercise — lower their risk of neurodegenerative disease or slow its progression.
In the study, published in Nature, the Stanford researchers compared blood samples from exercising and sedentary mice of the same age. They showed that transfusions of blood from running mice reduced neuroinflammation in the sedentary mice and improved their cognitive performance. In addition, the researchers isolated a blood-borne protein that appears to play an important role in the anti-neuroinflammatory exercise effect.
A protein of interest
Removing a single protein, clusterin, from marathoner mice’s plasma largely negated its anti-inflammatory effect on sedentary mice’s brains. No other protein the scientists similarly tested had the same effect.
Clusterin, an inhibitor of the complement cascade, was significantly more abundant in the marathoners’ blood than in the couch potatoes’ blood.
Further experiments showed that clusterin binds to receptors that abound on brain endothelial cells, the cells that line the blood vessels of the brain. These cells are inflamed in the majority of Alzheimer’s patients, noted Wyss-Coray, whose research has shown that blood endothelial cells are capable of transducing chemical signals from circulating blood, including inflammatory signals, into the brain.
Clusterin by itself, even though administered outside the brain, was able to reduce brain inflammation in two different strains of lab mice in which either acute body-wide inflammation or Alzheimer’s-related chronic neuroinflammation had been induced.
Separately, the investigators found that at the conclusion of a six-month aerobic exercise program, 20 military veterans with mild cognitive impairment, a precursor to Alzheimer’s disease, had elevated clusterin levels in their blood.
Wyss-Coray speculated that a drug that enhances or mimics clusterin’s binding to its receptors on brain endothelial cells might help slow the course of neuroinflammation-associated neurodegenerative diseases such as Alzheimer’s.
Wyss-Coray is a member of the Stanford Wu Tsai Neuroscience Institute, Stanford Bio-X, and the Stanford Maternal and Child Health Research Institute; and a faculty fellow of Stanford ChEM-H.
Conducting a Preclinical Assessment of a Compliance Matched Biopolymer Vascular Graft

Narrative heart disease is responsible for over 600,000 deaths annually, making it the number one killer of women and men in the United States. There are currently no small diameter vascular grafts that effectively treat this disease. McGowan Institute for Regenerative Medicine affiliated faculty member Jonathan Vande Geest, PhD, Professor, Department of Bioengineering, University of Pittsburgh, is the principal investigator on a project that will use computational tools to fabricate a fully biodegradable small diameter vascular tissue engineered graft that is and remains compliance matched as it remodels in-vivo.
The project, entitled “Preclinical Assessment of a Compliance Matched Biopolymer Vascular Graft,” will run for 4 years. The National Heart, Lung, and Blood Institute funded this project.
The abstract of the project follows:
There are approximately 250,000 coronary artery bypass graft (CABG) procedures performed annually to treat coronary heart disease (CHD) with graft failure rates reported to be as high as 42.8%. A major cause of graft failure in CABG has been attributed to graft compliance mismatch leading to subsequent intimal hyperplasia and graft thrombosis. The development of a compliance matched functional small diameter vascular graft will therefore significantly improve the treatment of those with CHD. Tissue engineering has shown promise in achieving some but not all of the required characteristics for a functional tissue engineered vascular graft (TEVG). A particularly challenging aspect in the development of a functional TEVG is the design of a fully biodegradable biopolymer graft that can be tuned to a desired compliance pre-implantation and subsequently maintain its compliance as it degrades and remodels in-vivo. As such there is a critical need to develop a compliance matched TEVG that remains compliance matched throughout the host remodeling process while also maintaining a functional endothelium. To meet this need we will develop and functionally assess a tropoelastin layered and endothelialized TEVG that is and remains compliance matched. We will utilize computational simulation to optimize the compliance of a biodegradable gelatin/tropoelastin layered TEVG that elutes TGFb2 in a controlled manner to promote early cell infiltration and late matrix deposition in our graft, thus stabilizing its compliance as our graft degrades. The overall working hypothesis of our research is that the intravital (in-vitro and in-vivo) compliance of our graft can be maintained by temporally controlling TGFb2 elution from a computationally optimized TEVG. We will test this hypothesis by completing the following Specific Aims. Aim 1 of our research project will assess if compliance and TGFb2 elution can maintain the compliance of our TEVG in-vivo using a rat aortic interpositional implantation model. Aim 2 of our proposed work will assess the function of our TEVG in a preclinical large animal (sheep carotid) implantation model. The proposed studies will establish a novel pre- and post-implantation compliance controlled fully biodegradable biopolymer TEVG with excellent patency, anti-thrombogenicity, vasoreactivity, and functional performance.
Fall 2021 Design Expo Showcases Engineering Undergrads Imaginative Designs
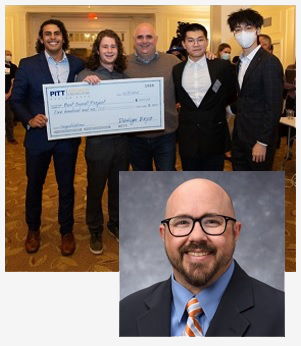
Each semester, students at the University of Pittsburgh Swanson School of Engineering get the chance to show off their creativity and highlight their designs at the Design EXPO, which was held in the University Club on Dec. 9, 2021. Students prepared their displays showcasing their work from the School’s Capstone Design courses or highlighted concepts and prototypes from the Product Realization, Medical Product Prototyping and Art of Making courses. The students presented their projects, and judges from industry visited the booths in turn to talk with students and view their work.
McGowan Institute for Regenerative Medicine affiliated faculty member Jonathan Vande Geest, PhD, Professor, Department of Bioengineering, University of Pittsburgh, served as a mentor on one project which took two of the winning prizes:
Best Overall Project and 1st Place Winner in the Mechanical Engineering and Materials Science Department
MEMS-5: Measurement Design and Optimization for Spring Cranioplasty in Craniosynostosis Patients
Academic Sponsors: Dr. Jonathan Vande Geest and Dr. Justin Beiriger
Students: Yuxuan Deng, Mazen Megahed, Henry Weinrieb, Zijie Xu
“Every semester, the Design EXPO is a chance for our students to recognize a problem or opportunity and apply the engineering skills they’re learning in the classroom to solve it, which is what engineering is all about,” said Mary Besterfield-Sacre, PhD, Associate Dean for Academic Affairs and Nickolas A. DeCecco Professor of Industrial Engineering. “I’m always impressed with the amazing projects these students bring to the table, and this year was no exception.”
Congratulations, all!
Illustration: The winning team of the Best Overall Project at the Fall 2021 Design EXPO: MEMS-5: Measurement Design and Optimization for Spring Cranioplasty in Craniosynostosis Patients. University of Pittsburgh Swanson School of Engineering.
Researchers Earn Charles E. Kaufman Foundation Grants

Pitt researchers have been awarded a portion of a $2.1 million grant for Pennsylvania universities from the Charles E. Kaufman Foundation. The foundation, established by chemical engineer and entrepreneur Charles E. Kaufman, supports fundamental scientific research in chemistry, biology, and physics at institutions throughout the commonwealth.
New Initiatives Research Grants, which carry an award of $300,000 over two years, are designed to encourage investigators with strong research records to establish interdisciplinary collaborations requiring expertise beyond a single researcher. Pitt recipients Nathan Lord, PhD, and Mo Ebrahimkhani, MD, will explore the elaborate language of signals used by human embryos and seek to decode the molecular language that enables embryos to control organ development in their project titled, “Spatially guided morphogenesis in human liver organoids.” This language tells each cell when and where to divide, migrate and differentiate, and this research seeks to systematically decode the molecular language that enables embryos to control organ development.
Dr. Lord is an assistant professor in the Department of Computational and Systems Biology in the School of Medicine, and Dr. Ebrahimkhani is an associate professor in the Department of Pathology, a member of the Pittsburgh Liver Research Center, and an affiliated faculty member of the McGowan Institute for Regenerative Medicine.
The foundation advisory board reviewed 121 inquiries from scientists at 23 colleges and universities. The latest awards will support research at the University of Pittsburgh, Bryn Mawr College, Bucknell University, Carnegie Mellon University, Drexel University, Haverford College, Pennsylvania State University, Swarthmore College, and Washington and Jefferson College.
Congratulations, Dr. Ebrahimkhani and Dr. Lord!
Precision Rehabilitation to Prevent Osteoarthritis

Athletes and sports fans know that a torn ACL knocks a player out of the game, requires surgical repair, and involves a long recovery. But for many injured athletes, being temporarily sidelined is only the beginning of what can become a lifelong struggle.
According to McGowan Institute for Regenerative Medicine affiliated faculty member Eni Halilaj, PhD, an assistant professor in mechanical engineering and a biomechanist at Carnegie Mellon University who specializes in orthopaedic rehabilitation, 60% of those who suffer this common knee injury also develop osteoarthritis early in life. The degenerative joint disease, which affects an estimated 32.5 million individuals in the U.S., is especially problematic for younger patients because of the longer time span during which the chronic condition can cause debilitating pain, stiffness, and limited mobility.
“How can we make the 60% have the same long-term outcome as the 40%?” asks Dr. Halilaj, who is working to understand the difference between those who do and those who do not develop osteoarthritis following knee trauma.
Dr. Halilaj and her interdisciplinary team of mechanical engineers, bioengineers, and computer scientists are working to integrate insights from their experimental and computational work to develop effective rehabilitation strategies aimed at restoring and preserving pain-free mobility throughout the lifespan.
Experiments in her motion capture laboratory focus on identifying mechanical risk factors for debilitating diseases like osteoarthritis. The 1,000-square-foot lab is outfitted with 20 cameras positioned along the ceiling throughout the room, which are used to visualize highly reflective spherical markers that are strategically placed on a human subject’s body to track their motion and analyze their gait. A split-belt treadmill further analyzes the subject’s motion by measuring the force exerted by each step. Electromyography (EMG) sensors are used to evaluate muscle activations during movement by measuring electrical activity produced by skeletal muscles.
While data gathered in this type of research lab is critical to identifying mechanical risk factors, patient access to such facilities is limited. Recent studies have shown that the presence of researchers observing gait analysis tests has a measurable effect on how the patients walk that could undermine the reliability of findings from traditional gait analysis studies.
The key to better insights may lie in monitoring how patients move in natural environments as opposed to specialized laboratories like Dr. Halilaj’s Musculoskeletal Biomechanics Lab.
“Using flexible wearable sensors that look like Band-Aids, we monitor movement outside of the lab, where patients are not on their best behavior and may be adopting pain avoidance walking strategies that damage their joints in the long run,” says Dr. Halilaj.
Her group is pairing wearable sensing data with advanced magnetic resonance imaging of the knee to discover the problematic walking strategies that are associated with early osteoarthritis—what she calls “digital biomarkers of osteoarthritis.”
In addition to gait adaptation following surgery, physical therapy plays an important role in recovery. Recent advances in computer vision now offer untapped potential for movement analysis from video, enabling real-time tracking and feedback to improve physical therapy. Dr. Halilaj and her team are also developing open-source software that fuses computer vision algorithms with biomechanical modeling to allow accurate motion tracking from inexpensive cameras, like those embedded in personal smartphones.
Observational studies that monitor patients in physical therapy and natural environments will help researchers like Dr. Halilaj discover digital biomarkers of future disease, which can be targeted with preventative technologies in the future. Together with experts in haptics, Dr. Halilaj’s team is developing wearable haptic systems to help train patients to change the way they move.
“In a not-too-distant future, we envision clinicians using data from these minimal wearables sensors and smartphone videos to isolate the 60% of patients who are likely to suffer from debilitating osteoarthritis, personalize their therapy accordingly, and even prescribe a wearable haptic device that helps them correct their gait before it is too late,” concludes Dr. Halilaj.
AWARDS AND RECOGNITION
Dr. Keith Cook Named Head of Biomedical Engineering at CMU

After a rigorous and extensive search domestically and internationally, McGowan Institute for Regenerative Medicine affiliated faculty member Keith Cook, PhD, has been selected to be the next head of the Biomedical Engineering Department (BME) at Carnegie Mellon University’s College of Engineering. The appointment takes effect immediately.
Dr. Cook joined Carnegie Mellon as a faculty member in 2013 and has been an outstanding researcher, as well as a strong advocate to build and advance the department. He has demonstrated his leadership skills by serving as the founding director of the Bioengineered Organs Initiative, and more recently he has taken the lead to form the Transforming Transplant Initiative.
In addition, Dr. Cook previously held the position of associate department head for graduate education and has played an active role in mentoring and supporting faculty development over the years. Most recently, he served as the interim head of BME since last February, adeptly advancing department priorities and skillfully navigating the challenges of the pandemic.
Congratulations, Dr. Cook!
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#229 –– Ms. Christine Kretz and Dr. William Wagner discuss biomanufacturing in low earth orbit with the International Space Station U.S. National Laboratory.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
PUBLICATION OF THE MONTH
Author: Junru Wu, Yoram Vodovotz, Sultan Abdelhamid, Francis X Guyette, Michael B Yaffe, Danielle S Gruen, Anthony Cyr, David O Okonkwo, Upendra K Kar, Neha Krishnamoorthi, Robert G Voinchet, Isabel M Billiar, Mark H Yazer, Rami A Namas, Brian J Daley, Richard S Miller, Brian G Harbrecht, Jeffrey A Claridge, Herbert A Phelan, Brian S Zuckerbraun, Pär I Johansson, Jakob Stensballe, James H Morrissey, Russell P Tracy, Stephen R Wisniewski, Matthew D Neal , Jason L Sperry, Timothy R Billiar, PAMPer study group
Title: Multi-omic analysis in injured humans: Patterns align with outcomes and treatment responses
Summary: Trauma is a leading cause of death and morbidity worldwide. Here, we present the analysis of a longitudinal multi-omic dataset comprising clinical, cytokine, endotheliopathy biomarker, lipidome, metabolome, and proteome data from severely injured humans. A “systemic storm” pattern with release of 1,061 markers, together with a pattern suggestive of the “massive consumption” of 892 constitutive circulating markers, is identified in the acute phase post-trauma. Data integration reveals two human injury response endotypes, which align with clinical trajectory. Prehospital thawed plasma rescues only endotype 2 patients with traumatic brain injury (30-day mortality: 30.3 versus 75.0%; p = 0.0015). Ubiquitin carboxy-terminal hydrolase L1 (UCHL1) was identified as the most predictive circulating biomarker to identify endotype 2-traumatic brain injury (TBI) patients. These response patterns refine the paradigm for human injury, while the datasets provide a resource for the study of critical illness, trauma, and human stress responses.
Source: Cell Rep Med. 2021 Dec 21;2(12):100478.
GRANT OF THE MONTH
PI: Jonathan Vande Geest
Title: Preclinical Assessment of a Compliance Matched Biopolymer Vascular Graft
Description: There are approximately 250,000 coronary artery bypass graft (CABG) procedures performed annually to treat coronary heart disease (CHD) with graft failure rates reported to be as high as 42.8%. A major cause of graft failure in CABG has been attributed to graft compliance mismatch leading to subsequent intimal hyperplasia and graft thrombosis. The development of a compliance matched functional small diameter vascular graft will therefore significantly improve the treatment of those with CHD. Tissue engineering has shown promise in achieving some but not all of the required characteristics for a functional tissue engineered vascular graft (TEVG). A particularly challenging aspect in the development of a functional TEVG is the design of a fully biodegradable biopolymer graft that can be tuned to a desired compliance pre-implantation and subsequently maintain its compliance as it degrades and remodels in-vivo. As such there is a critical need to develop a compliance matched TEVG that remains compliance matched throughout the host remodeling process while also maintaining a functional endothelium. To meet this need we will develop and functionally assess a tropoelastin layered and endothelialized TEVG that is and remains compliance matched. We will utilize computational simulation to optimize the compliance of a biodegradable gelatin/tropoelastin layered TEVG that elutes TGFb2 in a controlled manner to promote early cell infiltration and late matrix deposition in our graft, thus stabilizing its compliance as our graft degrades. The overall working hypothesis of our research is that the intravital (in-vitro and in-vivo) compliance of our graft can be maintained by temporally controlling TGFb2 elution from a computationally optimized TEVG. We will test this hypothesis by completing the following Specific Aims. Aim 1 of our research project will assess if compliance and TGFb2 elution can maintain the compliance of our TEVG in-vivo using a rat aortic interpositional implantation model. Aim 2 of our proposed work will assess the function of our TEVG in a preclinical large animal (sheep carotid) implantation model. The proposed studies will establish a novel pre- and post-implantation compliance controlled fully biodegradable biopolymer TEVG with excellent patency, anti-thrombogenicity, vasoreactivity, and functional performance.
Source: National Heart, Lung, and Blood Institute
Term: December 15, 2021 – November 30, 2025
Amount: $658,593 (one year)
