What’s Happening At The McGowan Institute?
June 2012 | VOL. 11, NO. 6 | www.mcgowan.pitt.edu
Bio-hybrid Device Acts as “Thermostat” to Control Systemic Inflammation in Sepsis
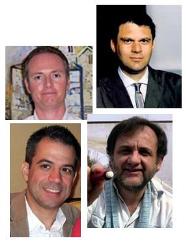 In a pre-clinical study by McGowan Institute for Regenerative Medicine faculty members and researchers from the University of Pittsburgh School of Medicine, a small, external bioreactor holding human cells pumped out an anti-inflammatory protein to prevent organ damage and other complications in a model of sepsis caused by bacterial products. The findings were published in the inaugural issue of Disruptive Science and Technology. The McGowan faculty members are (pictured top left clockwise):
In a pre-clinical study by McGowan Institute for Regenerative Medicine faculty members and researchers from the University of Pittsburgh School of Medicine, a small, external bioreactor holding human cells pumped out an anti-inflammatory protein to prevent organ damage and other complications in a model of sepsis caused by bacterial products. The findings were published in the inaugural issue of Disruptive Science and Technology. The McGowan faculty members are (pictured top left clockwise):
- Yoram Vodovotz, PhD, professor, Departments of Surgery, Immunology, Computational and Systems Biology, Clinical and Translational Science, and Communication Science and Disorders at the University of Pittsburgh, and director, Center for Inflammation and Regenerative Modeling at the McGowan Institute;
- Joerg Gerlach, MD, PhD, professor, Department of Surgery, University of Pittsburgh, and director, The Bioreactor Group at the McGowan Institute, and affiliated faculty members;
- Gregory Constantine, PhD, professor of mathematics and statistics at the University of Pittsburgh; and
- Ruben Zamora, PhD, research assistant professor at the University of Pittsburgh in the Department of Surgery.
Inflammation is a necessary biological response that brings cells and proteins to the site of tissue injury to contend with foreign agents, such as bacteria and the products they produce, and to begin the healing process, explained senior author Dr. Vodovotz. But sometimes, the inflammatory response escalates to create damage on its own, triggering more inflammation in a self-sustaining and dangerous cycle.
“In sepsis, for example, the inflammatory response evolves almost too quickly, but the available treatment strategies aim to prevent inflammation entirely,” he said. “A better approach would be to turn down the response when it’s too strong, yet still have appropriate inflammation signaling to promote tissue repair.”
During inflammation, the body makes a protein called tumor necrosis factor-alpha, or TNF-α. It also makes its counterpart, soluble TNF-α receptor, or sTNFR, which binds to and reduces the level of TNF-α. In some situations, such as sepsis, not enough sTNFR is made to limit the inflammatory response.
“This bio-hybrid device acts as a kind of inflammation thermostat,” Dr. Vodovotz said. “By loading it with cells that produce different amounts of sTNFR, or other inflammatory blockers, we may soon be able to tailor our interventions to carefully balance inflammation and immune responses based on the patient’s medical situation.”
His team is now exploring the effectiveness of cells engineered to produce sTNFR based on the individual production of TNF-α, rather than continuously, in order to create a disease-specific response for each patient. Such a personalized medicine therapy platform could be extended based on emerging knowledge regarding the biology of inflammation.
The Vodovotz group is also creating computer models of inflammation, which could be used to engineer the next generation of this device. The portability of the device could be particularly useful on the battlefield, where early intervention to control systemic inflammation after injury might improve the chances of survival.
SCIENTIFIC ADVANCES
Regenerative Medicine Spin Off Technology Moves Closer To Clinical Use
 A commercial version of technologies developed in the McGowan Medical Devices Prototype Laboratory (MMDPL) at the McGowan Institute for Regenerative Medicine has moved one step closer to serving the needs of patients with respiratory distress. ALung Technologies, Inc., a University of Pittsburgh licensee, presented an analysis of its recent clinical trial of the Hemolung Respiratory Assist System (RAS) (pictured) in patients with acute exacerbation of chronic obstructive pulmonary disease (COPD). The results of a clinical study in Germany were summarized in a paper that was presented at the 58th Annual Conference of the American Society of Artificial Internal Organs in San Francisco.
A commercial version of technologies developed in the McGowan Medical Devices Prototype Laboratory (MMDPL) at the McGowan Institute for Regenerative Medicine has moved one step closer to serving the needs of patients with respiratory distress. ALung Technologies, Inc., a University of Pittsburgh licensee, presented an analysis of its recent clinical trial of the Hemolung Respiratory Assist System (RAS) (pictured) in patients with acute exacerbation of chronic obstructive pulmonary disease (COPD). The results of a clinical study in Germany were summarized in a paper that was presented at the 58th Annual Conference of the American Society of Artificial Internal Organs in San Francisco.
The presentation, entitled “Extracorporeal CO2 Removal (ECCO2R) for Preventing Intubation in Patients with Exacerbated COPD: Results of the Hemolung Pilot Study,” was presented by McGowan Institute for Regenerative Medicine faculty member William Federspiel, PhD, the William Kepler Whiteford professor of bioengineering, chemical engineering, and surgery, University of Pittsburgh, the director of the MMDPL, and Chairman of ALung’s Scientific Advisory Board. The paper provided data from a subset of seven patients with acute exacerbation of COPD who were failing non-invasive ventilation and at a high risk of being intubated and placed on invasive mechanical ventilation. Patients in the study were provided ECCO2R with the Hemolung RAS to remove retained carbon dioxide. The study was led by principal investigator Prof. Dr. Felix Herth of the Thoraxklinik and University Hospital, Heidelberg, Germany.
In his presentation, Dr. Federspiel highlighted the improvement in respiratory status seen in these patients with severe exacerbations in which the Hemolung RAS was applied. Arterial pCO2 levels were reduced on average by 28% within 24 hours, leading to lessening dyspnea and improved clinical status. The device provided effective and stable CO2 removal on the order of 75 to 95 mL/min or up to approximately 50% of metabolic production. No unexpected adverse events were observed. All patients were able to avoid intubation while treated with the Hemolung RAS.
COPD afflicts over 14 million Americans and leads to nearly 140,000 deaths annually, making it the third leading cause of death. Acute exacerbations are a serious complication of COPD in which patients suffer a sudden worsening of their symptoms. In severe cases, patients will develop acute respiratory failure and require invasive mechanical ventilatory support. “These patients that go on to be mechanically ventilated often have a very poor prognosis with survival ranging from 31% to 76%,” said Dr. Nausherwan Burki, Professor of Medicine at the University of Connecticut Health Center and ALung’s Medical Director. “The ability of the Hemolung RAS to help patients with severe acute exacerbation of COPD to avoid intubation and invasive mechanical ventilation fills an important, unmet clinical need.”
“We are pleased to have completed our pilot study of the Hemolung RAS and to be progressing towards obtainment of the CE mark,” said Peter DeComo, ALung’s Chairman and CEO. “There is tremendous clinical enthusiasm for the Hemolung RAS, and we’re looking forward to introducing the product to key reference centers throughout Europe in the near future.”
Study: Intensivist Presence at Night Improves Patient Outcomes in ICUs with Limited Daytime Intensivist Staffing
 As a member of a study team, McGowan Institute for Regenerative Medicine affiliated faculty member Derek C. Angus, MD, MPH, professor and chair of the Department of Critical Care Medicine and Director of CRISMA (Clinical Research, Investigation, and Systems Modeling of Acute Illnesses) Center at the University of Pittsburgh, reported that intensive care units (ICUs) that have no or limited access to critical care doctors during the day can improve patient outcomes by having the specialists, called intensivists, staff the unit at night. However, the researchers were unable to find any incremental benefit of nighttime staffing in ICUs that were robustly staffed with the specialists during the day. The findings were published in the New England Journal of Medicine.
As a member of a study team, McGowan Institute for Regenerative Medicine affiliated faculty member Derek C. Angus, MD, MPH, professor and chair of the Department of Critical Care Medicine and Director of CRISMA (Clinical Research, Investigation, and Systems Modeling of Acute Illnesses) Center at the University of Pittsburgh, reported that intensive care units (ICUs) that have no or limited access to critical care doctors during the day can improve patient outcomes by having the specialists, called intensivists, staff the unit at night. However, the researchers were unable to find any incremental benefit of nighttime staffing in ICUs that were robustly staffed with the specialists during the day. The findings were published in the New England Journal of Medicine.
Research has shown that daytime staffing with intensivists improves ICU patient outcomes, noted senior author Jeremy M. Kahn, M.D., associate professor, Department of Critical Care Medicine, Pitt School of Medicine. But fewer than half of all ICUs in the U.S. are manned by intensivists, while many large medical centers, particularly teaching hospitals such as UPMC, have adopted not only intensivist staffing but have extended it to a 24-hour intensivist staffing model.
“Intuition would suggest that round-the-clock attention from an expert trained in critical care medicine would be of even greater benefit to these very ill patients,” Dr. Kahn said. “But until this project, no one had carefully examined whether that assumption would hold true. As it turns out, having some access to intensivists, who are in great demand, is the key to better outcomes. Round-the-clock intensivist staffing is only helpful in some ICUs.”
The research team reviewed admission details between 2009 and 2010 from 34 community and academic hospitals that use the Acute Physiology and Chronic Health Evaluation clinical information system, a database that collects details of patient outcomes as well as ICU staffing primarily for internal quality control monitoring. The researchers sent follow-up surveys to those hospitals and received responses from 25, which included 49 ICUs and nearly 66,000 patient admissions.
Dr. Kahn and his colleagues found that patient mortality was lower in ICUs where an intensivist was available at night only if there was no intensivist heavily involved in care during the day. In ICUs where intensivists were on duty during the day, mortality was unaffected by the presence of intensivists at night.
“There is a huge opportunity to improve survival rates in some ICUs by bringing an intensivist on board at night,” Dr. Kahn said. “However, there aren’t enough of us to staff all the ICUs that need intensivists, so hospitals with a strong intensivist presence during the day – like most academic medical centers – should consider whether additional intensivist coverage is needed at night.”
Agent That Can Block Fibrosis of Skin, Lungs Identified
 McGowan Institute for Regenerative Medicine affiliated faculty member Adriangina Larregina, MD, PhD, associate professor of the Departments of Dermatology and Immunology, University of Pittsburgh School of Medicine, along with fellow researchers at Pitt’s School of Medicine have identified an agent that in lab tests protected the skin and lungs from fibrosis, a process that can ultimately end in organ failure and even death because the damaged tissue becomes scarred and can no longer function properly.
McGowan Institute for Regenerative Medicine affiliated faculty member Adriangina Larregina, MD, PhD, associate professor of the Departments of Dermatology and Immunology, University of Pittsburgh School of Medicine, along with fellow researchers at Pitt’s School of Medicine have identified an agent that in lab tests protected the skin and lungs from fibrosis, a process that can ultimately end in organ failure and even death because the damaged tissue becomes scarred and can no longer function properly.
There are no effective therapies for life-threatening illnesses such as idiopathic pulmonary fibrosis and systemic sclerosis, which cause progressive organ scarring and failure, said senior author Carol A. Feghali-Bostwick, Ph.D., associate professor, Division of Pulmonary, Allergy and Critical Care Medicine, and co-Director of the Scleroderma Center, Pitt School of Medicine.
“It’s estimated that tissue fibrosis contributes to 45 percent of all deaths in developed countries because organ failure is the final common pathway for numerous diseases,” she said. “Identifying a way to stop this process from happening could have enormous impact on mortality and quality of life.”
The research team evaluated E4, a piece of protein or peptide derived from endostatin, a component of collagen known for its inhibition of new blood vessel growth. In lab tests, healthy human skin cells that were treated to become fibrotic remained normal when E4 was present. The skin and lungs of mice were protected from cell death and tissue scarring by a single injection of E4 administered 5 or 8 days after they were given the cancer drug bleomycin, which is known to induce fibrosis. The peptide also could reverse scarring that had already occurred, the researchers found.
In a unique approach, the investigators also tested E4 in human skin maintained in the laboratory to confirm it would be effective in treating fibrosis in a human tissue. E4 blocked new and ongoing fibrosis in human skin.
The agent might work by stalling the cross-linking of collagen needed to form thick scars, Dr. Feghali-Bostwick said. While the body naturally produces endostatin, it appears that it cannot make sufficient amounts to counteract fibrosis development in some diseases.
“This endostatin peptide passes two important hurdles that suggest it is a promising candidate drug for development for patients with idiopathic pulmonary fibrosis and systemic sclerosis” said Mark T. Gladwin, M.D., chief, Division of Pulmonary, Allergy and Critical Care Medicine at UPMC and Pitt. “It reverses established disease in animal models and it reverses fibrosis in the human skin fibrosis model.”
In a case of serendipity, the researchers discovered E4 while exploring the process of fibrosis. Post-doctoral fellow and study co-author Yukie Yamaguchi, M.D., Ph.D., was conducting some experiments with proteins thought to facilitate the scarring process.
“Dr. Yamaguchi showed me the tests that showed endostatin wasn’t working to increase fibrosis, but in fact shut it down,” Dr. Feghali-Bostwick said. “It was the opposite of what we expected and I was very excited about our finding. As Louis Pasteur once said, ‘chance favors the prepared mind.’”
AWARDS AND RECOGNITIONS
Dr. Savio Woo to Receive 2012 IEEE Medal for Innovations in Healthcare Technology
 McGowan Institute for Regenerative Medicine faculty member Savio L-Y. Woo, PhD, DSc, DEng, a world-leading bioengineer whose pioneering biomechanics research has profoundly impacted sports medicine and the management of ligament and tendon injuries leading to improved patient recovery, is being honored by the Institute of Electrical and Electronics Engineers (IEEE) with the 2012 IEEE Medal for Innovations in Healthcare Technology. IEEE is the world’s largest technical professional association.
McGowan Institute for Regenerative Medicine faculty member Savio L-Y. Woo, PhD, DSc, DEng, a world-leading bioengineer whose pioneering biomechanics research has profoundly impacted sports medicine and the management of ligament and tendon injuries leading to improved patient recovery, is being honored by the Institute of Electrical and Electronics Engineers (IEEE) with the 2012 IEEE Medal for Innovations in Healthcare Technology. IEEE is the world’s largest technical professional association.
The medal, sponsored by the IEEE Engineering in Medicine and Biology Society, recognizes Dr. Woo for pivotal contributions to biomechanics and its application to orthopedic surgery and sports medicine. The award will be presented at the IEEE Honors Ceremony in Boston, Massachusetts.
Dr. Woo is a pioneer in biomechanics known around the world for his over 40 years of translational research concerning the healing and repair of tissues. Biomechanics involves applying the engineering principles of mechanics to study body movement and the effects of forces acting on the musculoskeletal system. From research at the cellular and tissue level to developing computer and robotic models of joints, Dr. Woo, together with his 600 students, post-doctoral research fellows, and junior colleagues, has provided key insight to understanding the function of bone and connective tissue. His contributions have spurred advancements in the surgical treatment and rehabilitation of ligament and tendon injuries, ultimately leading sports medicine and orthopedic surgery into the 21st Century.
Dr. Woo helped develop the “controlled motion is good” concept, showing the benefits of joint movement and early weight-bearing activities during rehabilitation compared to immobilization following surgery. His approach to robotic testing of knee and shoulder movement helped define the beneficial effects of motion on healing. He applied computer modeling and robotic technology to study joint mechanics and the effects of injury on joint function. Dr. Woo used robots to produce motions that occur during everyday activities and to determine the forces that the motions generate in the ligaments of the joints. Dr. Woo’s work has resulted in much faster recovery time for patients with soft-tissue injuries. His methods also assist with surgical planning and can predict the success of surgical techniques.
Dr. Woo has also focused on using novel functional tissue engineering to heal and regenerate ligaments and tendons at the cellular, tissue, and organ levels using bioscaffolds. Bioscaffolds are small intestinal submucosa from genetically altered pigs that can be used to heal the anterior cruciate ligament of the knee. Dr. Woo is also leading the efforts of applying degradable metallic materials to regenerate ligaments and tendons severely damaged during sports injuries.
Dr. Woo began his career at the University of California, San Diego, as a professor of surgery and bioengineering in 1970 and moved to the University of Pittsburgh in 1990. In Pittsburgh, he founded the Musculoskeletal Research Center (MSRC) within the Departments of Orthopaedic Surgery and Bioengineering. The MSRC is a multidisciplinary education center where countless orthopedic surgeons, biologists, and bioengineering students have studied and worked.
Dr. Woo is a member of the U.S. Institute of Medicine, the U.S. National Academy of Engineering, and the Republic of China’s Academia Sinica. His honors include the H.R. Lissner Medal from the American Society of Mechanical Engineers (1991), the Muybridge Medal from the International Society of Biomechanics (1995), and the Olympic Prize for Sports Science from the International Olympic Committee (1998). Dr. Woo received his bachelor’s degree in mechanical engineering from California State University, Chico, and his master’s degree in mechanical engineering and doctorate in bioengineering from the University of Washington, Seattle. Dr. Woo is currently a Distinguished University Professor and Director of the Musculoskeletal Research Center within the University of Pittsburgh’s Department of Bioengineering and Swanson School of Engineering, Pittsburgh, Pennsylvania.
McGowan Institute for Regenerative Medicine 2012 Top Docs
 The McGowan Institute for Regenerative Medicine applauds its affiliated faculty members who were recently recognized by Pittsburgh magazine. Each year the magazine commissions Castle Connolly Medical Ltd. to select top doctors on the national and regional levels. The physician-led research team identifies highly skilled, exceptional doctors by evaluating their medical education, training, and hospital appointments, and by surveying area hospital leaders and physicians. This year 25 McGowan Institute affiliated faculty were recognized in the May issue of the magazine with three colleagues* receiving dual specialty acknowledgment. Congratulations are extended to:
The McGowan Institute for Regenerative Medicine applauds its affiliated faculty members who were recently recognized by Pittsburgh magazine. Each year the magazine commissions Castle Connolly Medical Ltd. to select top doctors on the national and regional levels. The physician-led research team identifies highly skilled, exceptional doctors by evaluating their medical education, training, and hospital appointments, and by surveying area hospital leaders and physicians. This year 25 McGowan Institute affiliated faculty were recognized in the May issue of the magazine with three colleagues* receiving dual specialty acknowledgment. Congratulations are extended to:
- Anesthesiology – Erin Sullivan, MD*
- Cardiovascular Disease – Michael Mathier, MD, Dennis McNamara, MD, David Schwartzman, MD
- Critical Care Medicine – Derek Angus, MD, MPH
- Gastroenterology – David Whitcomb, MD, MS, PhD
- Neurological Surgery – Douglas Kondziolka, MD, David Okonkwo, MD, PhD
- Ophthalmology – Joel Schuman, MD
- Orthopaedic Surgery – Freddie Fu, MD, James Kang, MD
- Otolaryngology – Barry Hirsch, MD, Clark Rosen, MD
- Pediatric Cardiac Surgery – Peter Wearden, MD, PhD
- Pediatric Cardiology – Jacqueline Kreutzer, MD
- Pediatric Cardiovascular Anesthesia – Erin Sullivan, MD
- Pediatric Neurological Surgery – Elizabeth Tyler-Kabara, MD, PhD
- Pediatric Urology – Steven Docimo, MD*
- Physical Medicine and Rehabilitation – Michael Boninger, MD
- Plastic Surgery – Howard Edington, MD*, Ernest Manders, MD
- Surgery – Timothy Billiar, MD, Abhinav Humar, MD, Ron Shapiro, MD
- Surgical Oncology – Howard Edington, MD
- Thoracic Surgery – Thomas Gleason, MD, James Luketich, MD
- Urology – Steven Docimo, MD
 Regenerative Medicine Podcast Update
Regenerative Medicine Podcast Update
The Regenerative Medicine Podcasts remain a popular web destination. Informative and entertaining, these are the most recent interviews:
#110 –– Dr. Beniash is an associate professor at the University of Pittsburgh School of Dental Medicine. His position is located in Oral Biology. Dr. Beniash discusses his research in biomineralization, the structure/function relationships in supramolecular assemblies, bioinspired materials, and tissue engineering.
Visit www.regenerativemedicinetoday.com to keep abreast of the new interviews.
Publication of the Month
| Authors: | Olton DY, Close JM, Sfeir CS, Kumta PN. |
| Title: | Intracellular trafficking pathways involved in the gene transfer of nano-structured calcium phosphate-DNA particles. |
| Summary: | Nano-structured calcium phosphate (NanoCaP) particles have been proven to be a powerful means of non-viral gene delivery. In order to better understand the mechanisms through which NanoCaPs-mediated mammalian cell transfection is achieved, we have sought to define the intracellular trafficking pathways involved in the cellular uptake and intracellular processing of these particles. Previous work has indicated that NanoCaP-DNA complexes are most likely internalized via endocytosis, however the subsequent pathways involved have not been determined. Through the use of specific inhibitors, we show that endocytosis of NanoCaP particles is both clathrin- and caveolae-dependent, and suggest that the caveolaer mechanism is the major contributor. We demonstrate colocalization of NanoCaP-pDNA complexes with known markers of both clathrin-coated and caveolar vesicles. Furthermore, through the use of quantitative flow cytometry, we present the first work in which the percent internalization of CaP-DNA complexes into cells is quantified. The overall goal of this research is to foster the continued improvement of NanoCaP-based gene delivery strategies. |
| Source: | Biomaterials. 2011 Oct;32(30):7662-70. Epub 2011 Jul 19. |
Grant of the Month
| PI | Alejandro Almarza and Stephen F. Badylak |
| Co-PI | Tim Maul |
| Title | A Regenerative Medicine Approach for TMJ Meniscus Restoration |
| Description | This proposal seeks support to investigate the use of a biologic scaffold composed of extracellular matrix (ECM) as an inductive scaffold for the in vivo generation of a temporomandibular joint (TMJ) meniscus. Strong pilot studies indicate that this inductive template can stimulate the endogenous formation of a fibrocartilaginous disc that closely mimics the composition, structure, and mechanical properties of native disc material. Approximately 3% to 4% of the population seeks treatment for TMJ disorders; 90% of which are women. Approximately 70% of patients with TMJ disorders suffer from disc displacement; a fact that identifies the TMJ disc as a critical component in the cascade of events that lead to TMJ pathology. Spontaneous TMJ disc regeneration in vivo does not occur, and subsequent articulate surface degeneration can lead to the need for total joint replacement with marked negative consequences upon the quality of life. Development of a replacement disc would protect articulate joint surfaces, mitigate morbidity, and obviate the need for subsequent joint replacement.
The central hypothesis of the proposed work is that constructive remodeling of an ECM scaffold toward a functional TMJ disc occurs as a result of recruitment of multipotential cells to the site of remodeling, modulation of the innate immune response, and that enhancement of the remodeling process can occur with associated mechanical preconditioning. In a focused 4-year study involving two Specific Aims, we will test this hypothesis. The first Specific Aim will determine whether controlled in vitro mechanical loading and seeding with a population of multipotential perivascular stem cells can enhance the ECM remodeling process. The second Specific Aim will compare the in vivo remodeling process of five different xenogeneic ECM constructs: 1) a non-crosslinked ECM scaffold, 2) a chemically cross-linked ECM scaffold, 3) a non-crosslinked cell seeded ECM scaffold, 4) a non-crosslinked, mechanically conditioned ECM scaffold, and 5) a non-crosslinked, cell seeded and mechanically conditioned scaffold. The temporo-spatial time course of remodeling will be determined and the relevance and importance of critical events at 4 separate time points post implantation: 2 weeks, 1, 3 and 6 months post implantation in a pig model of bilateral TMJ meniscectomy will be identified. This work is highly interdisciplinary and will utilize the ECM scaffold expertise of the Badylak laboratory, the mechanobiology expertise of the Almarza laboratory, and the surgical expertise of an accomplished oromaxillofacial surgeon to accomplish the Specific Aims. We have a biostatistician and a veterinary comparative anatomy consultant to complement our team. A clear timeline has been established and the studies are based upon solid preliminary data. |
| Source | National Institute of Dental & Craniofacial Research |
| Term | 07/01/2012 – 06/30/2013 |
| Amount: | Year 1 $628,939 Year 2 $628,939 Year 3 $634,550 Year 4 $634,550 |
Newsletter Comments or Questions: McGowan@pitt.edu
