The first known identification of two genes responsible for hypoplastic left heart syndrome (HLHS), a severe congenital heart defect, has been reported by researchers at the University of Pittsburgh School of Medicine. The findings are published today in the journal Nature Genetics. McGowan Institute for Regenerative Medicine affiliated faculty member Simon Watkins, PhD, Founder and Director of the Center for Biologic Imaging at the University of Pittsburgh, a member of the Pittsburgh Cancer Institute, and a Professor and Vice Chairman within the Department of Cell Biology, is a co-author on the study.
Congenital heart disease, or structural abnormalities in the heart that are present at birth, affect up to 1 percent of all live births. HLHS is a rare congenital heart disease where the left side of the heart is poorly developed, resulting in an inability to effectively pump blood to the rest of the body. It occurs in about 2 to 3 of every 10,000 live births in the United States, and is fatal if left untreated.
Current treatment for HLHS involves multiple complex surgeries in the first few years of a child’s life, and while effective in many patients, it does not improve heart function in many others. In those individuals, heart failure ensues and heart transplantation is required. The 5-year survival rate for HLHS patients is approximately 50 to 70 percent.
Though genetic risk factors are known to play a role in HLHS, specific genes have been hard to identify.
“Studying diseases with complex genetics is extremely challenging. Our study has been made possible by leveraging findings from a large-scale analysis in mice to recover mutations causing congenital heart defects. This resulted in the recovery of the first mouse models of HLHS. Analysis of these mice with HLHS allowed us to identify for the first time two genes interacting in combination to cause HLHS,” said Cecilia Lo, PhD, professor at Pitt’s School of Medicine who also holds the F. Sargent Cheever Chair in Developmental Biology. “By understanding the genetics and biology of HLHS, this can facilitate development of new therapies to improve the prognosis for these patients.”
Lo and her team used fetal ultrasound imaging to screen mice with experimentally induced mutations, looking for structural heart defects. From this screen, they recovered eight different mouse strains with structural and functional heart defects indicative of HLHS.
By comparing the genome of mice with the HLHS heart defects to the genome of normal mice, Lo and her team identified several hundred mutations in the HLHS mutant strains. Further analysis of these mutant mice indicated the genetic origins of HLHS likely involve many interacting genes. The relevance of these mutations was reinforced by the fact that many also were found in the same chromosomal regions previously shown to be associated with HLHS from human genetic studies.
Using CRISPR-Cas9 gene editing in mice, the researchers confirmed that mutations in these two genes can cause HLHS. Additionally, they sequenced 68 HLHS patient samples and found one individual with rare mutations in both SAP130 and PCDHA genes.
Molecular analysis showed that heart cells in affected animals were poorly developed and had mitochondrial defects, indicating that Sap130–Pcdha9 gene interactions play a crucial role not only in heart development but also in regulating metabolic function of the cardiac muscle.
These findings suggest HLHS may be associated with a fundamental cellular defect in the heart muscle that can compromise blood flow in patients. This has important therapeutic implications, as surgical repair will not be able to address the cellular muscle defect in HLHS patients, noted Lo.
The researchers are investigating other mutations identified through the genetic screen and plan to undertake more genetic analysis of HLHS patients to better understand the molecular and genetic factors that cause the disease.
Other study authors included researchers from Pitt, The Jackson Laboratory, University of Rochester School of Medicine and Dentistry, Cincinnati Children’s Hospital Medical Center, Children’s National Medical Center, Boston Children’s Hospital, University of San Diego School of Medicine, and Medical College of Wisconsin.
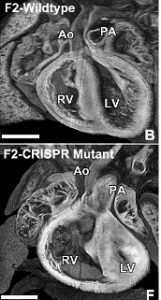
Illustration: Heart of CRISPR gene edited mice with HLHS (bottom) have a much smaller left ventricle (LV) compared to a normal mouse heart (top). Right ventricle (RV), Aorta (AO). Lo, et al.
Read more…
UPMC/University of Pittsburgh Schools of the Health Sciences Media Relations News Release
Abstract (The complex genetics of hypoplastic left heart syndrome. Xiaoqin Liu, Hisato Yagi, Shazina Saeed, Abha S Bais, George C Gabriel, Zhaohan Chen, Kevin A Peterson, You Li, Molly C Schwartz, William T Reynolds, Manush Saydmohammed, Brian Gibbs, Yijen Wu, William Devine, Bishwanath Chatterjee, Nikolai T Klena, Dennis Kostka, Karen L de Mesy Bentley, Madhavi K Ganapathiraju, Phillip Dexheimer, Linda Leatherbury, Omar Khalifa, Anchit Bhagat, Maliha Zahid, William Pu, Simon Watkins, Paul Grossfeld, Stephen A Murray, George A Porter Jr, Michael Tsang, Lisa J Martin, D Woodrow Benson, Bruce J Aronow and Cecilia W Lo. Nature Genetics; online May 22, 2017.)
