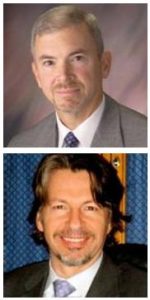
University of Pittsburgh School of Medicine researchers—including McGowan Institute for Regenerative Medicine affiliated faculty members Timothy Billiar, MD, George Vance Foster Endowed Professor and Chair in the Department of Surgery, and Derek Angus, MD, MPH, Distinguished Professor and the Mitchell P. Fink Endowed Chair of Critical Care Medicine—have demonstrated for the first time that changes over time in the volume of patients seen by trauma centers influence the likelihood of seriously injured patients living or dying.
The findings, reported online and scheduled for an upcoming issue of the journal Annals of Surgery, mean that changes in patient volume across all affected centers should be considered when designating a new trauma center in a region.
“It takes about three years for the impact of increased patient volume to translate into improved patient outcomes,” said lead author Joshua Brown, MD, MS, a research fellow in the Division of Trauma and General Surgery in the Pitt School of Medicine’s Department of Surgery. “Siphoning of patients through unregulated growth of unnecessary trauma centers can have a profound detrimental impact on patients that isn’t immediately obvious. Before designating a new trauma center, serious consideration should be given to how that designation will affect patient volumes over time at trauma centers throughout the region.”
A trauma center is a hospital equipped to immediately provide specialized care to patients suffering from major traumatic injuries, such as falls, car crashes, burns, or shootings. In the U.S., the American College of Surgeons sets criteria and conducts reviews for trauma center validation, and the individual states ultimately grant trauma center designation. In Pennsylvania, trauma centers are granted “Level” designations based on their capabilities, ranging from Level-I (highest) to Level-IV (lowest).
Dr. Brown and his colleagues examined records of nearly 840,000 seriously injured patients seen at 287 trauma centers between 2000 and 2012. The centers averaged 247 severely injured patients per year, and 90 percent of the cases involved blunt injury. The researchers compared the expected death rate for each center if everything involving each trauma patient’s care had gone perfectly to the center’s actual death rate.
Each 1 percent increase in patient volume at a trauma center was associated with 73 percent better odds of a patient surviving. Conversely, each 1 percent decrease in volume was linked to a two-fold worsening in the odds of a patient surviving.
“So, the study suggests the negative impact of declining patient volume is significantly greater than that of the positive impact of increasing patient volume,” said senior author Jason Sperry, MD, MPH, associate professor in the Pitt School of Medicine Departments of Surgery and Critical Care Medicine. “Granting unnecessary designation to a trauma center in a region that doesn’t have the patient volume to support it not only hurts patient outcomes at that new center, but it will likely lead to a decline in patient outcomes at other nearby centers.”
Follow-up study will be needed to determine why patient volume is linked to patient outcomes, but the researchers suspect that as centers increase their number of patients, they also increase their resources, infrastructure, and experience. Although advances in care and diagnostics may be more readily adopted at higher-volume trauma centers, this alone did not explain the influence of trauma center volume changes on patient outcomes over time.
“Taking care of patients who sustain complex traumatic injuries is a truly multidisciplinary effort, so it requires an institutional-level commitment of resources and staff,” said Dr. Brown. “There are many dynamics at play here that make the issue more involved than simply increased opportunity to hone surgical skills.”
Read more…
UPMC/University of Pittsburgh Schools of the Health Sciences Media Relations News Release
Abstract (Impact of volume change over time on trauma mortality in the United States. Brown, Joshua B. MD, MSc; Rosengart, Matthew R. MD, MPH; Kahn, Jeremy M. MD, MS; Mohan, Deepika MD, MPH; Zuckerbraun, Brian S. MD; Billiar, Timothy R. MD; Peitzman, Andrew B. MD; Angus, Derek C. MD, MPH; Sperry, Jason L. MD, MPH. Annals of Surgery; June 15, 2016.)
