The work of McGowan Institute for Regenerative Medicine faculty member Marina Kameneva, PhD, Research Professor of Surgery at the University of Pittsburgh School of Medicine, Professor of Bioengineering, University of Pittsburgh, and Director of the Artificial Blood Program at the McGowan Institute, and colleagues recently appeared in the May 31, 2017, online issue of the publication, Oncotarget. Co-authors on the paper are Samer Tohme, Hamza O. Yazdani, Vikas Sud, Julie Goswami, Patricia Loughran, Hai Huang Richard L. Simmons, and Allan Tsung, all of the University of Pittsburgh.
Dr. Kameneva’s article is entitled “Drag reducing polymers decrease hepatic injury and metastases after liver ischemia-reperfusion.”
The abstract reads:
Introduction: Surgery, a crucial therapeutic modality in the treatment of solid tumors, can induce sterile inflammatory processes which can result in metastatic progression. Liver ischemia and reperfusion (I/R) injury, an inevitable consequence of hepatic resection of metastases, has been shown to foster hepatic capture of circulating cancer cells and accelerate metastatic growth. Efforts to reduce these negative consequences have not been thoroughly investigated. Drag reducing polymers (DRPs) are blood-soluble macromolecules that can, in nanomolar concentrations, increase tissue perfusion, decrease vascular resistance and decrease near-wall microvascular concentration of neutrophils and platelets thereby possibly reducing the inflammatory microenvironment. We hypothesize that DRP can potentially be used to ameliorate metastatic capture of tumor cells and tumor growth within the I/R liver.
Methods: Experiments were performed utilizing a segmental ischemia model of mice livers. Five days prior or immediately prior to ischemia, murine colon adenocarcinoma cells (MC38) were injected into the spleen. DRP (polyethylene oxide) or a control of low-molecular-weight polyethylene glycol without drag reducing properties were administered intraperitoneally at the onset of reperfusion.
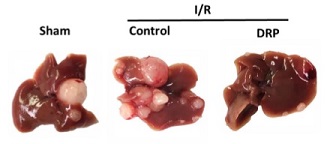
Results: After three weeks from I/R, we observed that liver I/R resulted in an increased ability to capture and foster growth of circulating tumor cells; in addition, the growth of pre-existing micrometastases was accelerated three weeks later. These effects were significantly curtailed when mice were treated with DRPs at the time of I/R. Mechanistic investigations in vivo indicated that DRPs protected the livers from I/R injury as evidenced by significant decreases in hepatocellular damage, neutrophil recruitment into the liver, formation of neutrophil extracellular traps, deposition of platelets, formation of microthrombi within the liver sinusoids and release of inflammatory cytokines.
Conclusions: DRPs significantly attenuated metastatic tumor development and growth. DRPs warrant further investigation as a potential treatment for liver I/R injury in the clinical setting to improve cancer-specific outcomes.
Illustration: After three weeks, I/R resulted in a significant increase in gross surface metastatic nodules compared with the sham groups (mean 12 nodules in I/R versus 4 nodules in sham; p < 0.001). Oncotarget.
Read more…
Paper (Drag reducing polymers decrease hepatic injury and metastases after liver ischemia-reperfusion. Samer Tohme, Marina V. Kameneva, Hamza O. Yazdani, Vikas Sud, Julie Goswami, Patricia Loughran, Hai Huang, Richard L. Simmons and Allan Tsung. Oncotarget; online 05-31-17.)
