A dislocated shoulder is a common sports injury that can occur with a single swing of the tennis racket or an awkward fall on the field. Though popping the bone back into the socket may seem like a simple solution, the reality is more complex.
The injury can sometimes require an operation, and improper surgical technique and healing can further exacerbate the injury. This puts individuals at increased risk for future dislocation or joint disease later in life.
To tackle this issue, multidisciplinary researchers from the University of Pittsburgh will use an award from the National Institutes of Health to study an individualized approach that may improve surgical outcomes and help athletes avoid lasting repercussions.
McGowan Institute for Regenerative Medicine affiliated faculty member Richard Debski, PhD, professor of bioengineering, and Albert Lin, MD, associate professor of orthopaedic surgery, will lead a study to improve injury assessment and repair using quantitative techniques to measure the magnitude and location of injury.
“Repair surgery has up to a 15 percent rate of failure, and these cases lead to instability and additional dislocations which limit the patient’s ability to return to an active life,” said Dr. Debski, who runs the Orthopaedic Robotics Laboratory at Pitt’s Swanson School of Engineering.
“Our research reveals this injury affects a larger region than previously thought and indicates that the location and magnitude vary from person to person,” he explained. “This suggests that an individualized approach may be more effective in treating dislocation injuries and improving surgical outcomes.”
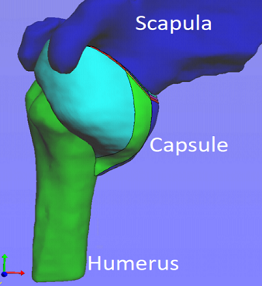
Dislocation injuries involve a sheet of soft tissue — called a capsule — that surrounds and stabilizes the joint. The high recurrence rate in capsular injuries can enlarge the damaged area, making a successful recovery even more difficult.
In this study, Drs. Debski and Lin will use a custom robotic system to dislocate a cadaveric shoulder and simulate clinical exams to assess joint stability. They will use an optical tracking system to measure the amount of permanent deformation or injury after each dislocation.
A surgeon will then perform a more precise repair procedure with the given location and magnitude of injury, and the results will be evaluated and compared to current methods.
“Despite significant advancement in surgical technique to address shoulder instability over the past 20 years, the rate of failure remains unacceptably high with real socioeconomic impact, particularly in a young patient population,” said Dr. Lin. “Dr. Debski and I have found that injury patterns vary significantly between patients; therefore, the key to improving recurrence rates may be individualized, anatomic surgeries specifically tailored to address the unique pattern injury rather than the current one-size-fits-all approach.”
Since the current optical tracking system cannot be used in a clinical setting, the team will also develop a new strategy to collect patient-specific measurements.
“We will use an MRI technique to characterize the injury and compare it to the quantitative patterns from our cadaveric model to see if there is a correlation between the data before and after surgical repair,” said Dr. Debski.
The findings of this study could validate the need for an individualized approach to capsular injury repair and potentially lead to a clinical trial.
“With this personalized approach, we hope to reduce the amount of failed capsular surgeries,” Dr. Debski said. “In the long run, we also hope to reduce the development of osteoarthritis in young adults, and ultimately, help these athletes make a healthy return to the sport that they love.”
Illustration: 3D model of MR arthrogram with division of the capsule into eight sub-regions. University of Pittsburgh Swanson School of Engineering.
Read more…
University of Pittsburgh Swanson School of Engineering News Release
