When a patient with heart disease is in need of a vascular graft but doesn’t have any viable veins or arteries in his or her own body, surgeons can rely on synthetic, tissue-engineering grafts. However, the body often treats these substitutes as a threat and rejects them. Researchers at the University of Pittsburgh are developing synthetic grafts that mimic the body’s own blood vessels to mitigate many of the complications of bypass surgery.
“The current best available treatment is to use the patient’s saphenous vein or mammary artery, but not everyone has enough of these healthy blood vessels to use when they need a bypass,” says McGowan Institute for Regenerative Medicine affiliated faculty member Jonathan Vande Geest, PhD, Professor of Bioengineering at Pitt’s Swanson School of Engineering. “A biocompatible, tissue-engineered graft would provide these patients with treatment options that currently do not exist.”
The National Institutes of Health awarded Dr. Vande Geest and his multi-institutional research team $672,682 for his one-year study, “Preclinical assessment of a compliance matched biopolymer vascular graft.” His research builds upon his work at Pitt’s Soft Tissue Biomechanics Laboratory designing newly engineered materials that mechanically and microstructurally behave the same way as the body’s native tissues.
“‘Biomimetic’ means that we study the organization and architecture of normal healthy tissue and use this information to guide our design and development of a tissue-engineered substitute,” explains Dr. Vande Geest. “For example, every functioning artery has a one-cell thick lining called an endothelium responsible for reducing thrombosis and controlling blood flow. Our graft will be endothelialized using blood derived endothelial cells.”
Large-diameter vascular grafts are commonly used in some vascular surgeries and can function perfectly up to 10 years after implantation. However, the body often treats small-diameter grafts as dangerous foreign objects. The result can be artery occlusion or blood clotting—detrimental conditions called hyperplasia and thrombosis, respectively.
“Small-diameter vascular grafts, or grafts involving blood vessels with an internal diameter smaller than five millimeters, have much higher failure rates than larger ones,” says Dr. Vande Geest. “A significant proportion of vascular disease cases involve small-diameter blood vessels, so the demand for viable treatment options is very high.”
A normal healthy artery is organized with alternating layers of collagen and elastin, which provide structural support and elasticity. Dr. Vande Geest’s proposed graft uses alternating layers of gelatin and tropoelastin as substitutes. Gelatin is derived from collagen, and tropoelastin is a precursor to elastin. He will use these materials along with computational optimization to engineer a graft with compliance similar to a real artery, eliminating compliance mismatch – an important rejection mechanism in currently used grafts.
“We believe our method of mimicking native artery microstructure and mechanics will result in a successful tissue-engineered graft, and this grant will support trials to perfect both our experimental and computational approach,” says Dr. Vande Geest.
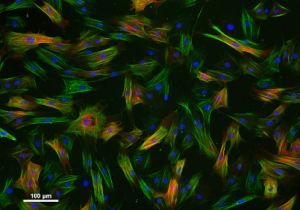
Illustration: Vascular smooth muscle cells.
Read more…
University of Pittsburgh Swanson School of Engineering News Release
