 Advanced age, being a man, and several types of preexisting health conditions have been associated with poor outcomes among hospitalized patients with COVID, but a new study suggests that other biological factors may be more important in determining prognosis and survival than these factors.
Advanced age, being a man, and several types of preexisting health conditions have been associated with poor outcomes among hospitalized patients with COVID, but a new study suggests that other biological factors may be more important in determining prognosis and survival than these factors.
Improved understanding of the biological underpinnings of different responses to SARS-CoV-2 infection could improve treatment for patients.
Most studies seeking to identify risk factors for COVID have grouped patients by age, sex, and preexisting conditions such as obesity, diabetes, and heart failure. “But that can potentially obscure contributions from underlying factors and obscure the potential that a single comorbidity can be associated with different outcomes,” says Soojin Park, MD, the study’s senior author, associate professor of neurology at Columbia University Vagelos College of Physicians and Surgeons, and a neurocritical care physician at Columbia University Irving Medical Center/NewYork-Presbyterian. Three McGowan Institute for Regenerative Medicine affiliated faculty members are co-authors of this study:
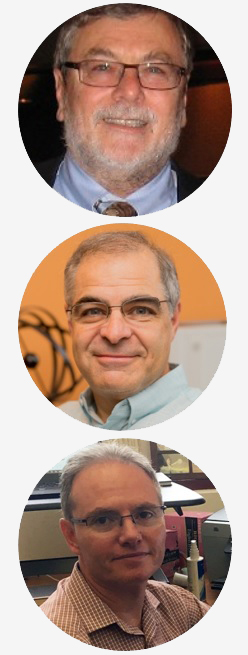
- Michael Pinsky, MD, professor of critical care medicine, bioengineering, cardiovascular diseases, clinical and translational science, and anesthesiology at the University of Pittsburgh
- Gilles Clermont, MD, a professor of critical care medicine, industrial engineering, and mathematics, and the medical director of the Center for Inflammation and Regenerative Modeling, University of Pittsburgh
- Yoram Vodovotz, PhD, professor of surgery, computational and systems biology, bioengineering, immunology, communication science and disorders (of the School of Health and Rehabilitation Science), clinical and translational science, and the director of the Center for Inflammation and Regeneration Modeling
To identify underlying factors that predict outcome, Dr. Park and her team used machine learning to analyze patient laboratory data collected throughout the hospitalizations of 528 patients treated at a single hospital during the first few months of the pandemic in 2020.
The analysis identified four unique groups of patients that had vastly different outcomes not expected based on classic risk factors such as age, sex, and preexisting conditions.
The group with the highest number of comorbidities, for example, did not have the worst outcomes and had a relatively low mortality rate, indicating that comorbidities alone are not responsible for variable COVID clinical courses.
The group of patients with the worst outcomes and most deaths had fewer comorbidities than expected but had higher levels of circulating inflammatory markers than the other three groups.
“Having certain high- or low-risk conditions does not guarantee a certain outcome,” says Dr. Park. “Rather, this highlights that healthy patients can still have poor COVID outcomes and patients with numerous chronic diseases can still have good outcomes.”
“Given the risk of poor outcome in a group of patients who were previously quite healthy, vaccination remains essential for everyone,” say Benjamin Ranard, MD, the study’s first author and a pulmonary and critical care fellow at Columbia.
Further examination of the different groups has potential to yield clinical and pathobiological insight into what is driving the vastly different clinical courses experienced by patients with COVID.
Read more…
Columbia University Irving Medical Center News Release
Abstract (Identification of endotypes of hospitalized COVID-19 patients. Benjamin L. Ranard, Murad Megjhani, Kalijah Terilli, Kevin Doyle, Jan Claassen, Michael R. Pinsky, Gilles Clermont, Yoram Vodovotz, Shadnaz Asgari and Soojin Park. Frontiers in Medicine, 11 November 2021.)
