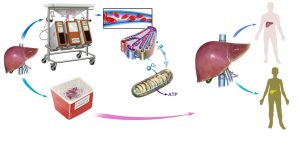
A new preservation system has been developed that pumps cooled, oxygen-rich fluid into donor livers not only keeps the organs in excellent condition for as long as 9 hours before transplantation, but also leads to dramatically better liver function. This system offers the potential to increase the survival of liver transplant recipients, according to a series of preclinical studies by researchers at the University of Pittsburgh School of Medicine and the McGowan Institute for Regenerative Medicine. The system could be tested with transplant patients at UPMC later this year.
 The findings, which were published online in the American Journal of Transplantation, suggest that it’s possible to use the technique of “machine perfusion” with a newly created cell-free oxygenated solution to expand the number of high-quality livers available for transplant, thereby shortening waiting times and reducing patient mortality.
The findings, which were published online in the American Journal of Transplantation, suggest that it’s possible to use the technique of “machine perfusion” with a newly created cell-free oxygenated solution to expand the number of high-quality livers available for transplant, thereby shortening waiting times and reducing patient mortality.
Currently, 20 to 40 percent of donor livers cannot be transplanted into recipients because oxygen deprivation during storage and transport in conventional containers can make pre-existing tissue damage worse, explained senior investigator Paulo Fontes, M.D., UPMC transplant surgeon, associate professor, Starzl Transplantation Institute, Department of Surgery, Pitt School of Medicine, and a deputy director of the McGowan Institute. If the damage is too extensive, the organ cannot be safely transplanted into a patient.
“Standard practice is to use a method called cold static preservation, which uses tissue cooling to slow down metabolism with the aim of reducing the demand for oxygen and thus protecting cells from death,” Dr. Fontes explained. “In our new system, we pump a special fluid designed to deliver oxygen to the liver, creating an environment that supports normal function. The integrity of the cells and vital metabolic activity is sustained for eventual transplantation of the organ.”
The research team optimized a machine-perfusion (MP) device that was developed by Organ Assist, a company in the Netherlands, and added a fluid with a hemoglobin-oxygen carrier component to deliver high concentrations of oxygen to the tissue. The liver is immersed in chilled fluid, which is also pumped through tubes inserted into the organ’s large blood vessels to effectively oxygenate the tissue.
The team transplanted six pigs with livers that had been kept for 9 hours, roughly the average time between recovery of the organ and transplantation into a recipient, in the MP system and another six with organs placed in the standard container.
They found that 100 percent of the pigs who got MP livers survived, compared to 33 percent of those who received conventionally preserved organs. The MP livers functioned better, produced more bile, and had higher oxygen levels than their conventional counterparts, and analyses of multiple biomarkers including inflammatory mediators indicated that the MP livers had been better preserved.
Also, “it was immediately obvious to us that the pigs who received MP livers looked much healthier and easily moved around their pens just hours after they woke up from the surgery,” Dr. Fontes said. “They didn’t look as ill as the animals treated with standard cold preservation. It was amazing.”
The data from the studies have been shared with federal regulators, he added, with the aim of launching a clinical trial to test the system at UPMC this year.
“This system has great potential to enhance our current standards for organ preservation, which should translate into more patients getting a life-saving procedure with potentially better outcomes,” Dr. Fontes said. “Not only that, we have hopes of a faster recovery because the liver could be less likely to become injured due to a lack of oxygen.”
Co-investigators include Roberto Lopez, M.D., Yoram Vodovotz, Ph.D., Ruben Zamora, Ph.D., Donna Stolz, Ph.D., Anthony Demetris, M.D., George Michalopoulos, M.D., Ph.D. (all McGowan affiliated faculty members of the McGowan Institute for Regenerative Medicine), Marta Minervini, Ph.D., Victor Scott, M.D., Kyle Soltys, M.D., Sruti Shiva, Ph.D., Shirish Paranjpe, Ph.D., David Sadowsky, Derek Barclay, and James Wallis Marsh, M.D., all of the University of Pittsburgh; and Arjan van der Plaats, Ph.D., of Organ Assist, Groningen, Netherlands.
